When Your Child Has Myasthenia Gravis (MG)
You have been told that your child has myasthenia gravis (MG). This condition makes your child’s muscles weak. MG is a serious condition. But it can be managed. With treatment, your child can still live an active and healthy life.
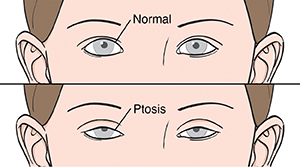 |
| Myasthenia gravis can cause symptoms such as droopy eyelids (ptosis). |
What causes MG?
Healthcare providers don't always know what causes MG. It happens due to problems with the connections between nerves and muscles. These are called neuromuscular junctions. With MG, the body’s immune system makes abnormal disease-fighting substances (antibodies) that attack at the neuromuscular junction. This stops the nerves from sending signals to the muscles they control. Then the muscles don't work properly.
Many experts believe that the most common forms of MG are not passed from parent to child (hereditary). But there is a form of MG where the antibodies are passed from mother (who has autoimmune MG) to infant. This often causes short-term (temporary) symptoms, which then go away. Infants with this form of MG don't have a higher risk for MG in the future. There is also a rare type of MG that is hereditary. With this type, a newborn develops symptoms that last their whole life.
What are the symptoms of MG?
The main symptom of MG is muscle weakness. This muscle weakness can range from mild to severe. Depending on which muscles are affected, MG may cause:
-
Droopy eyelids (ptosis)
-
Weak eye movements, which can cause double vision
-
Weakness in the neck, arms, and legs
-
Trouble speaking
-
Trouble chewing and swallowing
-
Trouble breathing
-
Trouble feeding (only infants)
-
Muscle weakness that increases during activity and improves after rest
How is MG diagnosed?
Your child will likely be referred to a pediatric neurologist. This is a healthcare provider with special training to find and treat problems that affect the nervous system in children. The healthcare provider will ask about your child’s health history and symptoms. The healthcare provider will also examine your child. Your child’s muscle strength will be tested. Skills such as vision, chewing, and swallowing will also be evaluated. Tests will be done to confirm the problem as well. These can include:
-
Nerve conduction study (NCS). This helps check nerve and muscle function. Electrodes (small round discs attached to wires) are placed on the skin over certain nerves and the muscles they control. A brief electrical current is sent to the nerves. The time it takes for the muscles to respond to the nerves is then recorded.
-
Electromyogram (EMG). This is often done with a nerve conduction study. It also helps check nerve and muscle function. Small needle electrodes are placed into muscles in the arms or legs. The electrical activity of the muscles is recorded when the muscles are active and when they are at rest.
-
Blood tests. These help check for certain cells or antibodies in the blood that are only present with MG. For these tests, a sample of blood is taken from a vein. Genetic tests may also be done if the hereditary type of MG is suspected.
-
Edrophonium test. This test helps check muscle strength. Medicine called edrophonium is injected into a vein. If your child has MG, the medicine will cause a brief increase in muscle strength. For instance, the eyelids may be less droopy for a short time.
How is MG treated?
Treatment for MG will vary for each child. The goal is to remove antibodies from the body. Treatments can include:
-
Medicines. These help improve muscle weakness. Some medicines treat the problems at the neuromuscular junction. Others help prevent the immune system from making abnormal antibodies.
-
Plasma exchange and high-dose IVIG. These treatments use special blood products. They help fight the body’s abnormal immune response or clear the abnormal antibodies from the bloodstream.
-
Surgery to remove the thymus gland. The thymus gland lies beneath the breastbone. It is involved in the immune system. In a person with MG, the thymus gland is more likely to be enlarged or abnormal. In some cases, removing the gland may improve symptoms or even make them go away. The healthcare provider will tell you more about this treatment if needed.
What are the long-term concerns?
MG is a long-lasting (chronic) condition. To help prevent problems, ongoing care is needed. This means your child needs regular checkups with the healthcare provider. Your child may also need to take medicines every day to help control symptoms. Your child may also be prescribed supportive care if needed. This can include speech, physical, or occupational therapy. Some children go into remission. This is a long period of having no symptoms.
People with MG are at risk for a medical emergency. Myasthenic crisis occurs when the lung muscles get so weak that they can't breathe on their own. Your child may need help breathing with a ventilator. This may be triggered as a side effect from a new medicine, stress, infections, or fever.
Coping with your child’s condition
Accepting your child’s diagnosis can be hard. Talking with a counselor may help you and your child work through your feelings. Joining a support group may also help. These groups let your child meet other children with MG. They also let you talk with other parents who are coping with their child having MG. MG support groups may be located through the Myasthenia Gravis Foundation of America ([email protected] or call 1-800-541-5454).