When Your Child Needs a Spinal Tap
A spinal tap (lumbar puncture) is a test that removes and checks a sample of CSF (cerebrospinal fluid). This fluid surrounds the brain and spinal cord.
During the test, a small sample of CSF is removed from the spinal canal. The sample is then studied in a lab. A spinal tap is relatively safe. There is a very small risk of infection or injuring the spinal cord or nerves. Within a few hours, your child’s body will make new fluid to replace what was removed. From start to finish, the test usually takes about 15 to 30 minutes. Some results will be available within hours. Other results will take a few days to finalize. This test is usually done to check for infection.
But there are other reasons to do a spinal tap. They can:
-
Check for bleeding in the brain
-
Look for cells that may mean your child has a central nervous system disease
-
Look for a tumor
-
Help diagnose multiple sclerosis, Guillain-Barré syndrome, or other neurological conditions
-
Deliver medicines such as chemo to the brain and spinal cord
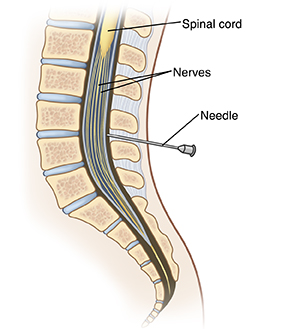 |
| During a spinal tap, a sample of cerebrosprinal fluid (CSF) is removed near the base of the spine. The spinal cord is not touched. |
Before the test
Follow all instructions given by your child’s healthcare provider to prepare your child for the test.
If general anesthesia will be used during the test, you’ll be given certain food, drink, and instructions for medicine to prepare your child. For instance, your child may be told to not eat or drink for a certain number of hours before the test.
Helping your child get ready
Many hospitals have people trained to help children cope with their medical care or hospital experience. These people are often called child life specialists. Check with your child’s healthcare provider if child life programs or other similar services are available. There are also things you can do to help your child get ready for a test or procedure. How best to do this depends on your child’s needs. Start with the tips below:
-
Use short and simple words to describe the test to your child. Tell them why it’s being done. Younger children tend to have a short attention span. So talk with them shortly before the test. Older children can be given more time to understand the test in advance.
-
Tell your child what to expect in the hospital during the test. For instance, you could talk about who will be doing the test and what the hospital room will look like.
-
Make sure your child understands which body parts will be involved in the test.
-
As best you can, describe how the test will feel. For instance, if your child is awake during the test, they may feel some mild pain or pressure when the needle is inserted. Let your child know that this mild pain won’t last long.
-
Let your child ask questions, and answer these questions truthfully. Your child may feel nervous or afraid. They may even cry. Let your child know that you’ll be nearby during the test.
-
Use play when telling your child about the test, if appropriate. With younger children, this can mean role-playing with a child’s favorite toy or object. With older children, it may help to read books or show pictures of what happens during the test.
Let the healthcare provider know
For your child’s safety and best results, tell the healthcare provider if your child:
-
Takes any prescription or over-the-counter medicines. This includes any medicines that may make your child more likely to bleed, such as aspirin or ibuprofen.
-
Is allergic to any medicines or iodine
-
Has any health problems, including conditions that may raise the risk for bleeding or increase pressure within the skull (intracranial pressure)
During the test
A spinal tap is done by a trained healthcare provider. Ask your child’s provider in advance if you can stay with your child in the hospital room. Your child may bring along a favorite toy, such as a stuffed animal, for comfort. At the time of the test, your child will:
-
Change into a hospital gown and lie on a hospital bed
-
Be given anesthesia, if needed. A trained nurse (anesthetist) or specialized provider (anesthesiologist) helps with this process. Special equipment is then used to closely monitor your child’s breathing, heart rate, and blood pressure.
-
Be asked to curl into a tight ball and then stay still, if they're going to be awake during the test
-
Have their lower back cleaned so that the skin is sterile
-
Get medicine to numb the area
-
Have the hollow needle inserted through their lower back into the small space that holds the fluid in the spinal canal. Sometimes the needle is inserted more than once to find the best place to draw the fluid. Once the needle is in place, the fluid sample is slowly collected. The pressure of the fluid may also be measured.
-
Have the needle removed once the fluid is collected. The area is then cleaned and bandaged.
Your child needs to lie still during the test. If this will be hard for your child, they may be given medicine (a sedative) ahead of time. This will help your child to stay calm during the test. General anesthesia is also an option. This is medicine that makes your child fall asleep and not feel pain during the test. Babies will need to be held in position by staff during the test. General anesthesia will be given in the operating room. Once the procedure is completed, your child will be taken to the postanesthesia care unit to be closely monitored as they wake up.
After the test
-
Your child may be asked to lie down, rest, and drink plenty of fluids for several hours before going home. Follow any activity restrictions given to you by your child’s healthcare provider.
-
Some soreness in the low back is normal. A headache is fairly common. A pain reliever, such as acetaminophen, may be recommended to help manage any discomfort. The healthcare provider may also recommend that your child rest lying down and drink plenty of fluids.
-
Schedule a follow-up appointment with your child’s healthcare provider to review the results of the test.
When to call your child's healthcare provider
Contact the healthcare provider if your child has any of the following:
-
Fever (see Fever and Children, below)
-
A seizure caused by fever
-
Your baby is fussy or cries and can't be soothed
-
A headache that is severe or lasts longer than 2 days
-
Muscle aches or lower back pain that is severe or lasts longer than 2 days
-
Leg tingling or weakness
-
Any change in behavior or activity level
-
Is confused or hard to wake up
-
Constant bleeding or clear fluid leaking from the needle site
-
Begins to act sicker or get worse
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use the rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below are guidelines to know if your young child has a fever. Your child’s healthcare provider may give you different numbers for your child. Follow your healthcare provider’s specific instructions.
Fever readings for a baby under 3 months old:
Fever readings for a child age 3 months to 36 months (3 years):
-
Rectal, forehead, or ear: 102°F (38.9°C) or higher
-
Armpit: 101°F (38.3°C) or higher
Call the healthcare provider in these cases:
-
Repeated temperature of 104°F (40°C) or higher in a child of any age
-
Fever of 100.4° (38°C) or higher in baby younger than 3 months
-
Fever that lasts more than 24 hours in a child under age 2
-
Fever that lasts for 3 days in a child age 2 or older