Understanding Acute Respiratory Distress Syndrome (ARDS)
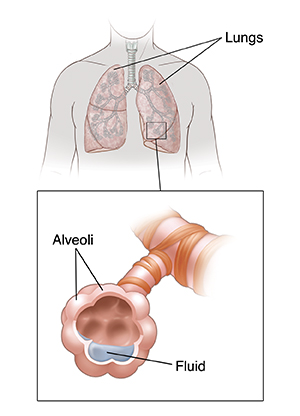
Acute respiratory distress syndrome (ARDS) is a severe lung condition. ARDS causes lungs to become inflamed and the small air sacs in the lungs (alveoli) to fill with fluid. The lungs then can’t work well enough to bring oxygen into the body. Most people with ARDS have so much trouble breathing that they need a machine (mechanical ventilator) to breathe for them.
What causes ARDS?
Experts don’t yet understand why ARDS occurs in some people and not in others. It can happen after an illness or injury, such as:
-
Viral infection, such as COVID-19 or flu
-
Severe body inflammation (sepsis)
-
Breathing stomach contents into the lungs (aspiration)
-
Breathing water into the lungs in a near-drowning
-
Lung infection, such as pneumonia
-
Chest injury that bruises the lungs
-
Breathing in smoke or other fumes
-
Severe burns or bleeding
-
Severe reaction to medicine, such as chemotherapy
-
Inflammation of the pancreas (pancreatitis)
-
Other severe injury
Certain things can make you more at risk for ARDS. These include:
Symptoms of ARDS
Symptoms often start 48 to 72 hours after the original illness or injury. They get worse quickly. They can include:
Diagnosing ARDS
Your healthcare provider will ask about your health history and give you a physical exam. They will listen to your lungs with a stethoscope as you breathe. A crackling sound may mean you have fluid in the lungs. You may have tests to check for signs of ARDS or other conditions that can cause fluid in the lungs. Tests may include:
-
Blood tests. These check your blood oxygen level and look for signs of infection.
-
Chest X-ray. This test can show fluid in the lungs.
-
Echocardiogram. This imaging test looks at the heart as it beats. It’s done to check for signs of heart failure.
-
Sputum culture. This test is done on mucus from your lungs. It checks for signs of lung infection, such as bacteria.
-
Lung biopsy. This procedure is rarely done during the diagnostic exam of people who may have ARDS.
Treatment for ARDS
The most common treatment for ARDS is mechanical ventilation. This means having a breathing machine send oxygen-rich air into your lungs. A tube is put through your mouth and throat, and down into your lungs. The tube is connected to a machine called a ventilator that gives you air. It can be adjusted to give you as much air as needed. You may need to be on a ventilator for a week or more.
You'll also likely be given medicine to keep you relaxed (sedated) and relieve pain while the tube is in your throat. This is because the tube is uncomfortable, and you need to not move too much while it’s in place. In some cases, a tube may be put through a small cut (incision) in the front of your throat. This is called a tracheostomy. This can be more comfortable and allow for less sedation while you’re on the breathing machine. This is often done after the breathing tube has been in your throat for several days.
Some patients are treated with extracorporeal membrane oxygenation when a ventilator alone is not effective. This machine works like an artificial lung. It removes carbon dioxide from the blood and returns oxygenated blood back to the body.
You'll also be given other types of treatment that may include:
-
Liquid nutrition through a tube that leads to your stomach
-
Liquid nutrition through a tube put in a vein in your chest or arm
-
Antibiotics to treat an infection
-
Diuretic medicine to help remove extra fluid from your body
-
Medicine to prevent blood clots or stomach bleeding
-
Noninvasive ventilation such as through a BiPAP or CPAP machine
Because ARDS can be a life-threatening condition, you may need other tests and to make decisions about your care in a short period of time. Your healthcare team will keep you and your family informed of your condition. They will let you and your family know the treatments being used or considered. They can answer your questions and concerns.
When you start to recover, you will be weaned off the ventilator. This means less air will be used and your lungs will do more work. Weaning is done carefully over days. The breathing tube is removed when your lungs are working well enough.
Possible complications of ARDS
ARDS can cause scarring of the lungs (fibrosis). It can cause organ failure from lack of oxygen to the organs. It can also cause death.
Preventing ARDS
You can lower your risk for ARDS by:
-
Staying up-to-date on vaccines, such as for flu and COVID-19. Ask your healthcare provider which are right for you.
-
Don't smoke. Ask your healthcare team for help quitting.
-
Limit alcohol. Men should have no more than 2 drinks per day. Women should have no more than 1 drink per day.
-
Limit exposure to pollution if possible.
Life after ARDS
Recovery from ARDS can take time. After ARDS, you may have problems, such as less lung function. You may feel weak and get tired more easily. You may need to use oxygen at home. You may also need other home-based services, such as physical and occupational therapy. You may have depression and anxiety, or problems with thinking and remembering. ARDS can cause emotional stress for both the person and their family. Talk with the healthcare team about treatment for depression and anxiety. Also ask about counseling and ARDS support groups for you and your family. You should see a healthcare provider who has experience with ARDS for follow-up care.
Call 911
Call 911 right away if you have these symptoms after an illness or injury:
-
Shortness of breath
-
Fast breathing
-
Fast heart rate
-
Chest pain
-
Blue, purple, or gray color of nails and lips
-
Unable to talk
-
Feeling faint or dizzy
-
Coughing or as directed by your healthcare provider
-
Fever of 100.4°F (38°C) or higher, or as directed by your healthcare provider
-
Chills or as directed by your healthcare provider