Having Pneumatic Retinopexy
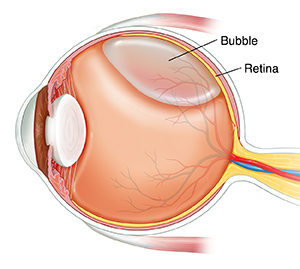
Pneumatic retinopexy is a procedure to correct a detached retina. It helps to bring back vision. It uses a special tool to fix the retina and a small bubble of gas to hold the retina in place so it can heal.
What to tell your healthcare provider
Tell your healthcare provider about all the medicines you take. This includes over-the-counter medicines such as ibuprofen. It also includes vitamins, herbs, and other supplements. And tell your healthcare provider if you:
-
Have had any recent changes in your health, such as an infection or fever
-
Are sensitive or allergic to any medicines, latex, tape, or anesthesia (local and general)
-
Are pregnant or think you may be pregnant
Tests before your procedure
You will need some exams before your procedure. Your healthcare provider may use special tools to shine a light in your eye and look at your retina. You will need to have your eyes dilated for the eye exam. You also may have an ultrasound of your eye. This test helps your healthcare provider look at the detached retina.
Your healthcare provider may also do other tests to better understand your condition.
Getting ready for your procedure
Talk with your healthcare provider about how to get ready for your procedure. You may need to stop taking some medicines before the procedure, such as blood thinners and aspirin. If you smoke, you may need to stop before your procedure. Smoking can delay healing. Talk with your healthcare provider if you need help to stop smoking.
Also make sure to:
-
Ask a family member or friend to take you home from the hospital. You can't drive yourself.
-
Follow any directions you are given for not eating or drinking before your procedure.
-
Follow all other instructions from your healthcare provider.
-
Tell your provider if you have any concerns about keeping your head in a certain position for a long period of time after the procedure. You may need to do so to help with your recovery.
You will be asked to sign a consent form that gives your permission to do the procedure. Read the form carefully. Ask questions before you sign if something is not clear.
On the day of your procedure
The procedure is done in an eye care provider’s office. Your healthcare provider will tell you what to expect during your procedure. A typical procedure goes like this:
-
You will likely be awake during the surgery. You may get medicine to help you relax. The healthcare provider will use anesthetic eye drops to make sure you don’t feel anything. Your healthcare provider may inject another anesthetic around your eye.
-
The healthcare provider will use eye drops to dilate your pupil. It will stay dilated for several hours after the procedure.
-
Your healthcare provider may use a syringe to remove some fluid from inside your eye.
-
Your healthcare provider will inject a bubble into the area near your retina. They will use an ophthalmoscope to make sure the air bubble is in the right place.
-
Once your provider is sure that the bubble is in the correct place, they will check your vision, the blood flow in your retina, and your eye pressure.
-
Your healthcare provider will put antibiotic ointment on your eye. This is to help prevent infection.
-
A patch may be put on your eye.
After your procedure
Ask your healthcare provider about what you should expect after your procedure. Plan to have someone go home with you after the procedure.
Follow your healthcare provider’s instructions about eye care. You may need to take eye drops with antibiotics to help prevent infection. Your eye may be a little sore after the procedure, but you should be able to take over-the-counter pain medicines. You may need to wear an eye patch for a day or so.
Recovering at home
Follow your healthcare provider’s instructions about how to position your head after the procedure. This will help to prevent problems. You may need to keep a certain position for 8 hours per day or more for a week or 2 after your procedure. Doing so helps keep the gas bubble in place, making sure that your retina stays attached in the correct position. If you have concerns about keeping your head in a certain position for a long period of time, tell your healthcare provider before consenting to the procedure.
You should not travel by airplane or go to a higher elevation until the gas bubble has gone away. Ask your healthcare provider when it will be safe for you to fly again. You may also need to limit your activities until the gas bubble in your eye is completely gone. This may include no strenuous exercise or heavy lifting. Talk with your provider about when you can resume your normal activities.
Follow-up care
You will need close follow-up care with your healthcare provider to see how the procedure worked. You may have an appointment the day after the procedure. You may have appointments for the first few weeks after the procedure for close monitoring. If the procedure doesn’t work, you may need to have surgery.
When to call your healthcare provider
Call your healthcare provider right away if you have any of these:
-
Decreased eyesight
-
Eye swelling that gets worse
-
Eye pain that doesn’t get better or gets worse
-
Any new floaters, flashes of light, or other changes in your vision, such as a shadow or curtain
-
Any sign of infection, such as increased pain, swelling, or redness around the eye