Whipple Procedure
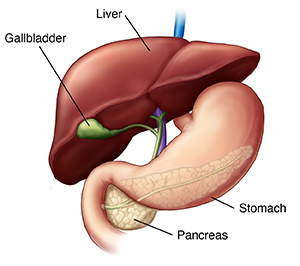
The Whipple procedure is also called pancreaticoduodenectomy. During this surgery, parts of the pancreas, small intestine, and other organs are removed. It's done to treat cancer of the pancreas. The pancreas is a gland attached to the small intestine. It makes digestive enzymes and sends them into the intestine to help digest food. It also makes insulin, a hormone that controls the body’s sugar level.
The surgery is most often done to treat cancer near the head (widest part) of the pancreas. It's usually done only if the cancer hasn't spread to other parts of the body (metastasized). But it may also be done to relieve or prevent symptoms (palliation). The procedure may also be done for other conditions such as:
-
Painful chronic pancreatitis that doesn't respond to other treatments.
-
Benign pancreatic lesions.
-
Cancers in the bile duct.
-
Cancers in the small intestine.
-
Severe pancreatic trauma.
-
Pancreatic cysts.
The surgery takes at least 5 hours. You'll likely need to stay in the hospital for 1 to 2 weeks afterward.
Before the surgery
Your doctor may have you follow a special clear-liquid diet for 1 to 2 days before the surgery. Also, you’ll have to stop taking medicines such as blood thinners and aspirin. And you may be told to take a laxative.
During the surgery
A needle is placed in a vein in your hand or arm. It’s attached to a tube called an IV line. The IV line gives you fluids and medicine to prevent pain. This may include a sedative or anesthesia. Depending on the medicine used, you may be drowsy or asleep during the surgery. Medicine may also be put into your back to numb you from the waist down.
Open surgery: The surgeon will make a cut in your belly (abdomen). If the surgery is for cancer, the surgeon will examine your pancreas and abdomen. This is to check the size and location of the cancerous tumor. The surgery will continue only if the tumor can be removed safely. The surgeon may also continue the surgery if they feel that it can relieve or prevent your symptoms.
If the open surgery proceeds, it involves two phases.
-
Phase one: The surgeon removes the head of the pancreas. Because the pancreas is so closely tied with other organs, the surgeon may remove other nearby organs. These include a section of the small intestine, the gallbladder, and part of the common bile duct, part of the stomach, and nearby lymph nodes. In some cases, the body of the pancreas is also removed.
-
Phase two: The remaining part of the pancreas and the common bile duct are connected to the intestine. The intestine is then reconnected to the stomach. This restores the pathway for food from the stomach to the remainder of the small intestine, and then to the large intestine.
When the open surgery is done, the surgeon closes the incision with sutures or staples. You will have tubes in your incisions called drains. These are usually in place for a few days. You may also have a tube in your nose that goes to your stomach. This drains fluid for a few days. You may also have a tube in your bladder that will drain the urine for a few days.
Laparoscopic surgery: The surgeon makes small cuts (incisions) in the belly. A thin tube with a lighted camera at its tip is inserted through one incision. The surgeon operates using specially designed surgical instruments placed through the remaining incisions.
Robotic surgery: The surgeon operates through several small incisions. Robotic arms equipped with special instruments and a tiny camera are used.
To decide which method is best for you, discuss all of the options with your surgeon.
After the surgery
You’ll be taken to the post-anesthesia care unit (PACU) or intensive care unit (ICU). Nurses will closely watch your condition. You’ll be moved to a hospital room when you’re stable. You'll get medicines to help manage pain and relieve symptoms. When you are able, you will be urged to get up and walk. This helps prevent lung and blood flow problems. You won’t be able to eat for a few days. You’ll receive nutrition through your IV. Several days after surgery, you will start on a liquid diet. You will then slowly return to your normal diet. Before you go home, make sure you have all the medicines and home care instructions you'll need.
Risks and possible complications
All surgeries have risks. The risks of this procedure include:
-
Infection.
-
Bleeding.
-
Pain.
-
Leakage of the connection between the intestine and the bile duct, pancreas, or stomach.
-
The surgery fails to resolve the problem.
-
A small possibility of developing diabetes. Or if you have diabetes, it may become worse.
-
Developing chronic diarrhea from loss of digestive hormones.
-
Leg swelling or blood clots.
-
Complications from anesthesia.
-
Death.
Recovering at home
Follow all instructions from your doctor after you are back at home. Make sure to:
-
Take all medicines as directed. Take pain medicines on time. Don’t wait until pain is bad to take them.
-
Care for your incision as instructed. This includes keeping the it clean and dry, especially when bathing or showering. Don't take tub baths until your doctor says it's OK.
-
Don't lift anything heavy or do strenuous activities.
-
Walk at least a few times daily. Slowly increase your pace and distance, as you feel able.
-
Don't drive until your doctor says it's OK and you're not taking pain medicines.
-
Keep in mind that recovery from major surgery takes time. You'll have good days and bad days. Don’t push yourself too hard.
Follow-up
Keep all follow-up appointments with your doctor. If you had cancer, your doctor will discuss any other treatments you need. You may need to take supplements that contain pancreatic enzymes for a while after the surgery.
When to call the health care provider
Call your doctor right away if:
-
You have a fever of 100.4°F (38°C) or higher, or as advised by your doctor.
-
You have chills.
-
You have increased redness, pain, swelling, bleeding, or drainage from any incisions.
-
You are vomiting.
-
You have too much bloating.
-
You don't have bowel movements.
-
Your stools are oily or loose.
-
You have jaundice (a yellow tint to the skin or eyes).
Call 911
Call 911 right away if: