When Your Child Has Acute Bronchitis
Acute bronchitis occurs when the bronchial tubes (airways in the lungs) become infected or inflamed. Normally, air moves in and out of these airways easily. When a child has acute bronchitis, the tubes become narrowed, making it harder for air to flow in and out of the lungs. This causes shortness of breath and coughing or wheezing. Acute bronchitis often goes away without treatment in a few days to a few weeks.
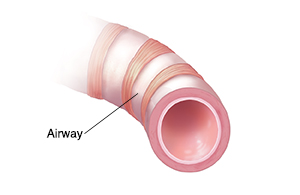 |
| A healthy airway allows a clear passage for air. |
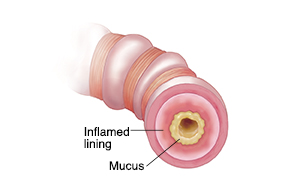 |
| An inflamed airway blocks airflow. |
What causes acute bronchitis?
-
A cold, the flu, or other common respiratory viruses
-
A bacterial infection
-
Exposure to irritants such as tobacco smoke, smog, paint, and household cleaners
-
Other respiratory problems, such as asthma
What are the symptoms of acute bronchitis?
Acute bronchitis often comes on suddenly, often after a cold or the flu. Symptoms include:
-
Noisy breathing or wheezing.
-
Mucus buildup in the airways and lungs.
-
Slight fever and chills.
-
Shortness of breath.
-
Feeling tired (fatigue).
-
Sucking in of the skin around the ribs when your child inhales (chest retractions), a sign of difficult breathing.
-
Coughing up yellowish-gray or green mucus.
How is acute bronchitis diagnosed?
Your child’s health history, a physical exam, and certain tests can help your child’s health care provider diagnose bronchitis. During the exam, the provider will listen to your child’s chest and check their ears, nose, and throat. One or more of these tests may also be done:
-
Sputum culture. This laboratory test looks for germs in the sputum, which is the material coughed out from the air passages when a person coughs deeply. Based on your child's age, this test may be optional because it is hard to do in younger children.
-
Chest X-ray. Your child may have a chest X-ray to look for an infection in the lungs (pneumonia).
-
Other tests. Your child may have other tests to check for underlying problems such as allergies or asthma. Your child may be referred to a specialist for these tests.
How is acute bronchitis treated?
The best treatment for acute bronchitis is to ease symptoms. Antibiotics are often not helpful because viruses cause most cases of acute bronchitis. To help your child feel more comfortable:
-
Give your child plenty of fluids, such as water, juice, or warm soup. Fluids loosen mucus, helping your child breathe more easily. They also prevent dehydration.
-
Make sure your child gets plenty of rest.
-
Keep your house smoke-free.
-
Consider using “children’s strength” medicine for symptoms. Talk about all over-the-counter products with the health care provider before you use them, including cough syrup. The U.S. Food and Drug Administration (FDA) advises not using cough or cold medicine in children younger than age 2. And manufacturers have labeled these cough and cold products to state: “Do not use in children under 4 years of age.” Also, use caution when giving these medicines to kids ages 4 to 11. Discuss the medicines with your child's provider.
-
Don’t give aspirin (or medicine that contains aspirin) to a child younger than age 19 unless directed by your child’s provider. Taking aspirin can put your child at risk for Reye syndrome. This is a rare but very serious disorder. It most often affects the brain and the liver.
-
Never give ibuprofen to an infant 6 months old or younger.
-
If you have questions or concerns, always check with your child's provider or pharmacist before giving your child any medicines.
If antibiotics are prescribed
Your child’s health care provider will prescribe antibiotics only if your child has a bacterial infection. In that case:
-
Make sure your child takes all the medicine, even if they feel better. Otherwise, the infection may come back.
-
Be sure that your child takes the medicine as directed. For example, some antibiotics should be taken with food.
-
Ask your child’s provider or pharmacist what side effects the medicine may cause and what to do about them.
-
If your child develops side effects, contact your child's provider before you give another dose.
Preventing future infections
To help your child stay healthy:
-
Teach children when and how to wash their hands. It’s the best way to prevent most infections.
-
Don’t let anyone smoke in your house, car, or around your child. Don't take your child to places where people smoke.
-
Keep your child up-to-date on recommended vaccines. Ask your child's health care provider what vaccines your child needs and when they should get them. This may include the influenza (flu) vaccine. The shot is advised for young children because they are especially at risk of flu, which can lead to bronchitis.
Tips for correct handwashing
Use clean, running water and plenty of soap. Work up a good lather.
-
Clean the whole hand, under the nails, between fingers, and up the wrists.
-
Wash for at least 20 seconds (as long as it takes to say the ABCs or sing “Happy Birthday” twice). Don’t just wipe—scrub well.
-
Rinse well. Let the water run down the fingers, not up the wrists.
-
In a public restroom, use a paper towel to turn off the faucet and open the door.
-
If there isn't water and soap available, use hand sanitizer with at least 60% alcohol.
When to get medical care
Contact the health care provider if your otherwise healthy child has:
-
Fever (see "Fever and children" below).
-
Symptoms that get worse or new symptoms.
-
Symptoms that don’t start to get better in a week, or within 3 days of taking antibiotics.
-
Bronchial infections that keep coming back.
Call 911
Call 911 if your child has any of these:
-
Trouble breathing
-
Skin sucking in around the ribs when your child breathes in (retractions)
-
Blue, purple, or gray skin color, especially lips
-
Trouble talking or swallowing
-
Loss of consciousness or dizziness
-
Seizure-like activity
-
Shortness of breath or wheezing
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The health care provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use a rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel okay using a rectal thermometer, ask the provider what type to use instead. When you talk with any provider about your child’s fever, tell them which type you used.
Below is when to contact the provider if your child has a fever. Your child’s provider may give you different numbers. Follow their instructions.
When to contact a health care provider about your child’s fever
For a baby under 3 months old:
-
First, ask your child’s health care provider how you should take the temperature.
-
Rectal or forehead: 100.4°F (38°C) or higher
-
Armpit: 99°F (37.2°C) or higher
-
A fever of ___________as advised by the provider
For a child age 3 months to 36 months (3 years):
-
Rectal or forehead: 102°F (38.9°C) or higher
-
Ear (only for use over age 6 months): 102°F (38.9°C) or higher
-
A fever of ___________ as advised by the provider
In these cases:
-
Armpit temperature of 103°F (39.4°C) or higher in a child of any age
-
Temperature of 104°F (40°C) or higher in a child of any age
-
A fever of ___________ as advised by the provider