When Your Child Has Hives (Urticaria) or Angioedema
Hives (urticaria) are raised, red, itchy bumps on the skin. Each bump can last for a few hours or days and then go away completely. Groups of hives can come and go for days at a time in different parts of the body. Hives can be uncomfortable. But they won’t harm your child or leave scars. Hives are not contagious. Sometimes your child may have severe swelling around the face, lips, throat, or eyes. This is a more serious skin reaction called angioedema. It can happen with hives or on its own.
What causes hives?
Hives often develop when cells in your child’s skin release a chemical called histamine during an allergic reaction. The histamine produces swelling, redness, and itching. Here are some of the most common causes of hives:
-
Food allergies. Common foods that may cause an allergic reaction include peanuts, shellfish, tree nuts, eggs, and milk. Food additives such as monosodium glutamate (MSG) and artificial colorings can also cause a reaction.
-
Viral infections
-
Prescription and over-the-counter (OTC) medicines. These include antibiotics (such as penicillin), sulfa-containing antibiotics, anticonvulsant medicines, phenobarbital, aspirin, and ibuprofen.
-
Extreme heat or cold:
-
Emotional stress
-
Scratching the skin, continual striking of the skin, or wearing tight-fitting clothes that rub the skin (dermatographism)
-
Exercise or physical activity
-
Bug bite or stings
-
In some cases, hives keep coming back, but there is no known cause (chronic urticaria).
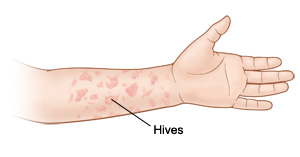
What do hives look like?
Hives are raised itchy bumps that can vary in color from pink to deep red. They come in different sizes. They sometimes spread to form large patches of swollen skin. Hives can appear on one part of the body and disappear on another in a few hours. Hives usually clear up within 24 hours. But new hives may keep forming for days or even weeks.
How are hives diagnosed?
Your child’s healthcare provider can diagnose hives by looking at your child’s skin and taking a full health history. Your child may also have skin tests. These look for foods or other substances that your child may be sensitive to. Blood tests may be done to rule out causes of hives not linked to allergies. But in most cases, the cause is never found.
How are hives treated?
For mild symptoms:
-
Give your child an oral over-the-counter antihistamine. Diphenhydramine can help, but it can cause drowsiness. Because of that,it's usually recommended at bedtime. Cetirizine, fexofenadine, loratadine, or levocetirizine may help during the day because these medicines are less likely to cause drowsiness. Talk with your child's healthcare provider about which medicine is best for your child.
-
To ease itching and swelling, use calamine lotion or cool compresses. Or have your child soak in a cool bath. (Adding 2 cups of ground oatmeal to the tub may make your child more comfortable).
For more severe symptoms, your child’s healthcare provider may prescribe:
-
A prescription or OTC oral antihistamine. It blocks the chemical in the body that causes allergic reactions. Your child is likely to take it every 4 to 6 hours for a few days. Some antihistamines may make your child drowsy. Some work faster than others. Ask your child’s provider which antihistamine to use and the correct dose to give your child.
-
An oral steroid to ease severe hives or swelling. It’s often taken for 3 to 5 days.
-
Epinephrine (adrenaline) to use in an emergency to stop a severe allergic reaction. If swelling affects your child’s breathing, call 911 right away. Your child is likely to need epinephrine to stop the allergic response.
Angioedema
Angioedema is a type of allergic reaction. It sometimes happens along with hives. It causes swelling deep in the skin. This occurs especially around the face, lips, throat, and eyes. Swelling that happens in the throat can make it hard to breathe. If this happens, call 911 right away.
Staying safe
To help prevent hives, stay away from any substances your child is sensitive to.
-
If your child has food allergies, read labels carefully. And be careful in restaurants.
-
Tell your child’s healthcare provider, dentist, and pharmacist about any allergies your child has to medicines. Keep a list of alternate medicines handy.
-
Talk to your child's teacher if food precautions need to be taken at school.
-
If your child has ever had a severe allergic reaction, ask your provider about carrying epinephrine and developing an Anaphylaxis Action Plan. This plan, prescribed by your physician, describes the symptoms of anaphylaxis and the actions to take.
-
Educate your child's teacher and appropriate school personnel to the Anaphylaxis Action Plan and the prescribed emergency epinephrine.
-
Have your child wear a medical alert bracelet.
Call 911
Call 911 right away if your child has any of these:
-
Wheezing, or trouble breathing or swallowing
-
Swelling of the lips, tongue, or throat
-
Dizziness or fainting
-
Loss of consciousness
-
Stomach pain, cramps, vomiting, diarrhea, or bloating
-
Constant coughing
-
Feeling of doom
Online Medical Reviewer:
Jessica Gotwals RN BSN MPH
Online Medical Reviewer:
Marianne Fraser MSN RN
Online Medical Reviewer:
Rita Sather RN
Date Last Reviewed:
7/1/2023
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.