Transurethral Resection of the Prostate (TURP)
TURP is surgery to treat a noncancer (benign) enlargement of the prostate. This condition is called BPH (benign prostatic hyperplasia). TURP removes prostate tissue to ease pressure on the urethra. This helps ease symptoms such as:
-
Urinary blockage
-
Frequent urination
-
Weak urine stream
TURP is one of the most common procedures for treating BPH. But some other procedures also help ease BPH symptoms. Your healthcare provider may do 1 of these instead of TURP. They include:
-
TUIP (transurethral incision of the prostate)
-
TUNA (transurethral needle ablation)
-
Laser ablation
-
Microwave therapy
-
UroLift system (uses permanent implants to lift and move prostate tissue blocking the urethra)
-
Rezum procedure (a water-vapor treatment that uses steam to reduce the size of the prostate)
Your healthcare provider can tell you more about these procedures. Your preparation and experience during surgery will be similar to the TURP procedure.
Getting ready for surgery
Your healthcare provider will tell you how to get ready for your procedure.
-
Tell you provider about any medicines you take. These include prescription and over-the-counter medicines. They also include vitamins, herbs, and supplements. You may be asked to stop taking certain medicines a few days before the procedure.
-
Follow all directions you're given for not eating or drinking before the surgery.
-
Follow all other instructions you’re given.
-
You will be asked to read and sign a form called an informed consent. This form explains the risks and benefits of the procedure. And it gives the provider your permission to proceed. Be sure all of your questions are answered before you sign.
During the TURP procedure
-
You'll be given medicine (anesthesia) to keep you pain-free during surgery. It may be given into your spine (epidural). This isn't meant to put you to sleep. But it will numb the area where the surgery is being done. In some cases, general anesthesia is used. This will let you comfortably sleep during the entire procedure. The anesthesia provider will explain the anesthesia that will be used. They will talk with you about the post-procedure pain medicine that's best for you.
-
The surgeon puts a long, thin tube with a light at the end (cystoscope) into your urethra. This tube lets them see the blocked part of the urethra.
-
A cutting tool is put into the tube. This is used to remove the extra prostate tissue that is causing pressure on the urethra. This excess tissue collects in the bladder and is washed away with fluids during the surgery.
-
These tissue samples are sent to a lab. There they are checked under a microscope to be sure they're cancer-free.
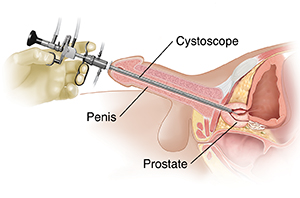 |
| Excess prostate tissue is removed during a TURP to let urine flow freely through the urethra. |
Possible risks and complications of prostate procedures
-
Bleeding
-
Infection
-
Scarring of the urethra
-
Retrograde ejaculation (see below)
-
Can’t get or keep an erection (rare)
-
Fluid is absorbed during the procedure (TURP syndrome)
-
Lifelong incontinence (very rare)
Retrograde ejaculation
After some surgical treatments, you may have retrograde ejaculation. This is when semen goes into the bladder during ejaculation, instead of out of the penis. So there may be little or no semen when you ejaculate. You may not be able to have children (infertility). If you plan to have children, talk with your healthcare provider before having the TURP procedure. Otherwise, this isn't harmful to your bladder. You'll still be able to have an erection and feel an orgasm. Retrograde ejaculation can also be a side effect of certain medicines.
Online Medical Reviewer:
Marianne Fraser MSN RN
Online Medical Reviewer:
Raymond Kent Turley BSN MSN RN
Online Medical Reviewer:
Rita Sather RN
Date Last Reviewed:
4/1/2024
© 2000-2025 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.