When Your Child Has Pneumothorax
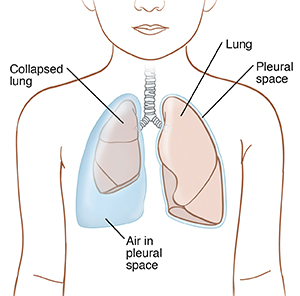
The space between the lung and chest wall is called the pleural space. Pneumothorax occurs when air leaks out of the lung and is trapped in this space. The air presses on the lung and can cause part or all of the lung to collapse.
What causes pneumothorax?
There are several types of pneumothorax. Each type has a different cause. The types are:
-
Traumatic pneumothorax. This type occurs when an injury damages the lung and causes a leak. The injury may be due to such things as a blow, fall, car accident, or broken rib.
-
Primary spontaneous pneumothorax. This type occurs when there is a weakened spot (bleb) on the surface of the lung. Most children with blebs have no related health problems and no symptoms. But if a bleb ruptures, pneumothorax results.
-
Secondary spontaneous pneumothorax. This type is due to lung disease. It is more likely to occur in children with problems, such as cystic fibrosis or asthma.
-
Iatrogenic pneumothorax. This type develops as a complication of another medical procedure. These can include central venous line placement (when a large IV is placed in a vein in the upper chest or neck) and mechanical ventilation using a ventilator.
What are the symptoms of pneumothorax?
Symptoms of pneumothorax vary for each child. The most common symptoms include:
-
Sharp, stabbing type chest pain that may spread to the shoulder and back
-
Shortness of breath or trouble breathing
-
Fast, shallow breathing
-
Dry cough
-
Tiredness
In more severe cases, symptoms can also include:
How is pneumothorax diagnosed?
The healthcare provider will examine your child, and listen to your child’s heart and lungs through a stethoscope. The healthcare provider will also keep an eye on your child's oxygen levels. This is done by using a monitor connected to sticky pads on your child's finger or toe, or with blood tests. A chest X-ray will be done to see how severe the leak is. In some cases, a CT scan or an ultrasound may also be done. These tests combine X-rays, computer scans, and sound waves to provide detailed pictures of the lungs.
How is pneumothorax treated?
The healthcare provider will monitor your child’s symptoms. Your child will be given breathing support with oxygen, and by a ventilator if needed. Any underlying health problems or injuries can be identified and treated.
If the leak is small and your child’s symptoms are under control, your child may be sent home without any further treatment. A small pneumothorax usually heals on its own. However, it's more common for children to stay overnight in the hospital to make sure that the pneumothorax does not grow in size and need further treatment.
If the leak is large, your child will be admitted to the hospital. One or more of these treatments may then be done:
-
Aspiration. A needle is inserted between the ribs into the pleural space. This helps remove the leaked air, so breathing can return to normal.
-
Chest tube placement. A thin tube is placed between the ribs and into the pleural space. The tube is then left in place. This tube is attached to a suction device that removes the leaked air. This helps the lung expand fully again. The tube may be left in place for a few days while the leak in the lung heals.
-
Surgery. This may be done if other treatments fail to close the leak. It may also be done if your child has had more than one pneumothorax. During surgery, blebs may be removed or sealed off. Methods may also be used to make the surface of the lung thicker and harder to rupture. The healthcare provider will tell you more about surgery for your child if it is needed.
What are the long-term concerns?
Most children do well after treatment. But they are at increased risk of having another pneumothorax in the future. To help prevent recurrence, your child may be advised not to do certain activities, such as scuba diving and frequent air travel. Children with lung disease are at higher risk to have continued problems after treatment. They will need regular visits to their healthcare provider to manage their health and condition.
Call 911
Severe pneumothorax can be fatal if not treated. Call 911 right away if any of the following occur:
-
Sudden, sharp, stabbing chest pain. It may spread to the shoulder and back, and it gets worse with deep breaths or coughing.
-
Severe shortness of breath or trouble breathing
-
Bluish color to the skin, from lack of oxygen
-
Fainting
-
Fast heartbeat
Online Medical Reviewer:
Amy Finke RN BSN
Online Medical Reviewer:
Jessica Gotwals BSN MPH
Online Medical Reviewer:
Liora C Adler MD
Date Last Reviewed:
5/1/2022
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.