Overactive Bladder Syndrome (OAB)
When the bladder muscles squeeze (contract) involuntarily, it's called overactive bladder syndrome (OAB). This causes an intense urge to pee, called urgency. Urgency can occur many times during the day and night. If urine leaks with the urgency, it is called urge incontinence.
A disease that affects the bladder nerves, such as multiple sclerosis, can cause overactive bladder syndrome. Other conditions can also lead to OAB. These include urinary tract infection (UTI) or prostate problems in men. But the exact cause is often not known.
OAB is not a normal part of aging. If you have symptoms, seek medical treatment.
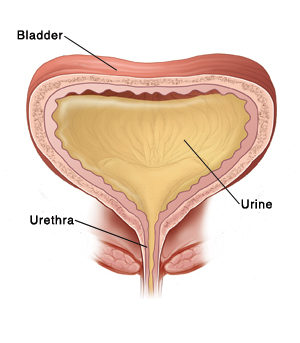 |
| Normally, urine stays in the bladder until a person decides to release it. With OAB, the bladder muscles contract involuntarily, causing a sudden urge to urinate and even urine leakage. |
How is overactive bladder syndrome diagnosed?
Your healthcare provider will examine you and ask about your symptoms and health history. You may also have one or more of these tests:
-
Urine test. Urine samples are taken and checked for problems, especially signs of infection.
-
Urinary diary. You record how much fluid you take in and pee out for 3 days.
-
Bladder ultrasound. This studies the bladder as it empties. Ultrasound uses sound waves to make detailed images of the inside of the body.
-
Cystoscopy. This test lets the provider look for problems in the urinary tract. The test uses a thin, flexible scope (cystoscope) with a light and camera on the end. The scope is put into the tube that takes urine out of the body (urethra).
-
Urodynamic studies. This is a group of tests. They measure and record many aspects of urinary bladder function. This includes pressures, volume, and urine flow.
How is overactive bladder syndrome treated?
Treatment depends on the cause and severity of your OAB. Treatments may include:
-
Changing your peeing habits. Your healthcare provider may advise certain methods, such as delayed voiding or timed urination.
-
Making dietary changes. Stay away from certain foods and drinks that are known to irritate the bladder. These include caffeine, alcohol, spicy foods, citrus foods, and chocolate.
-
Exercising your pelvic muscles. This can help strengthen pelvic muscles used when you pee. These exercises are called Kegels. They include contracting as if you were stopping your urine stream. And tightening your rectum as if trying not to pass gas. Your provider can help you learn how to do Kegels.
-
Biofeedback. This can help you learn to control the movement of your bladder muscles. Sensors are placed on your belly. They turn signals given off by your muscles into lines on a computer screen.
-
Medicine. This may be given to relax the bladder muscle. Medicine can also help ease bladder contractions. This reduces the urge to urinate. You may need to take medicine for months or years.
-
Neuromodulation. This may be done if medicine and behavioral changes don’t work. Electrical pulses are sent to the nerves that affect the pelvic area (sacral nerves). These pulses help relieve OAB and urge incontinence.
-
Botulinum toxin shots. These can be injected into the muscle of the bladder to relax the muscles.
-
Surgery. When less invasive treatments don't work, surgery to make the bladder larger may be done in severe cases.
With treatment, OAB can be managed. You may need to continue muscle-strengthening exercises and make changes in your daily routine. This may include going to the bathroom more often than you think you need to or developing a timed schedule. Your healthcare provider can tell you more.
When to call your healthcare provider
Call the healthcare provider right away if you have any of these:
-
Fever of 100.4° F ( 38°C ) or higher, or as directed by your provider
-
Symptoms don't get better, or get worse with treatment
-
Trouble peeing because of pain
-
Back or belly pain
Online Medical Reviewer:
Marianne Fraser MSN RN
Online Medical Reviewer:
Raymond Kent Turley BSN MSN RN
Online Medical Reviewer:
Rita Sather RN
Date Last Reviewed:
8/1/2023
© 2000-2025 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.