Ileus
Ileus occurs when there is a problem with motility in the stomach and small or large intestine (bowel). Motility is the movement of food and waste through the digestive tract. Ileus is not caused by a physical blockage (obstruction).
Normally, muscles in the bowel walls squeeze (contract) to move waste along. Signals from nerves tell the muscles when to contract. With ileus, this movement slows down or stops completely. As a result, waste can’t move through the bowels and out of the body. This can cause belly (abdominal) pain and other symptoms. Treatment is needed to restore normal movement and ease symptoms.
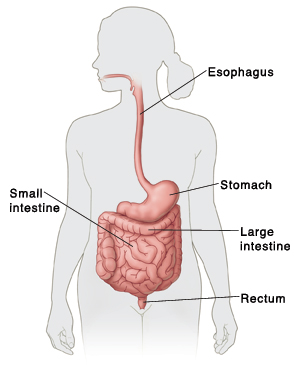 |
| The digestive tract. |
Causes of ileus
Ileus can be caused by:
-
Abdominal surgery
-
Abdominal infection
-
Injury to blood vessels that supply blood to the abdomen
-
Low levels of sodium or potassium (electrolyte imbalance)
-
Certain medicines, such as opioid pain medicines
-
Certain kidney or lung diseases
-
Certain health problems, such as cystic fibrosis and diabetes
Symptoms of ileus
Common symptoms of ileus include:
-
Belly swelling or bloating
-
Upset stomach (nausea) and vomiting
-
Belly cramps
-
Constipation or diarrhea
-
Loss of appetite
-
Not able to keep food down
-
Not able to pass stool or gas
Diagnosing ileus
Your healthcare provider will ask about your symptoms and health history. You’ll also have a physical exam. If your provider thinks you may have ileus, you may have tests to confirm the problem. These can include:
-
Imaging tests. These provide pictures of the bowels. Common tests include X-rays and a CT scan.
-
Blood tests. These are done to check for infection and other problems, such as fluid loss (dehydration).
-
Upper GI (gastrointestinal) series. This test takes X-rays of the upper digestive tract, from the mouth to the small intestine. An X-ray dye (contrast fluid) is used. The dye coats the inside of the upper digestive tract. This makes it show up clearly on X-rays.
Treating ileus
In most cases, ileus goes away by itself when the main cause clears up. The goal is to manage symptoms until movement in the digestive tract returns to normal. Treatment takes place in a hospital. As part of your care, the following may be done:
-
No food or drink is given by mouth usually for 24 to 72 hours. This allows your bowels to rest.
-
An IV (intravenous) line is placed in a vein in your arm or hand. The IV line is used to give fluids (hydration). It may also be used to give medicines. You may need medicines to improve movement in your digestive tract, or to ease pain. You may also need them to treat any underlying infections or conditions you have.
-
A soft, thin, flexible tube (nasogastric tube) is inserted through your nose and into your stomach. The tube is used to remove extra gas and fluid in your stomach and bowels. This helps to ease symptoms, such as pain and swelling.
-
You’ll be watched closely in the hospital until your symptoms get better. Your provider will tell you when you’re well enough to go home. This is often in a few days.
-
In rare cases, problems may occur. Other treatments, such as surgery, may then be done. Your provider will tell you more about other treatments, if needed.
Preventing ileus after surgery
After surgery, your healthcare team will work hard to prevent you from getting an ileus. They may:
-
Help you get up soon after surgery to move around. This promotes bowel movement. Your team will make sure your pain is managed well so you can get up soon after surgery.
-
Keep track of you closely for an ileus. This includes listening to the sounds in your belly (your "bowel sounds") to make sure your bowels are starting to work normally again.
-
Limit how much fluids and foods you eat until they know your bowels are starting to work again.
Your healthcare team will give you specific instructions depending on the type of surgery you had. Follow their instructions.
Long-term concerns
After treatment, most people fully recover. In some cases, you may need to see your provider for a follow-up appointment.
When to call the healthcare provider
Call your healthcare provider right away if you have any of these:
-
Fever of 100.4°F (38°C) or higher, or as advised by your provider
-
Chills
-
Belly swelling or pain that won’t go away
-
Not able to pass stool or gas
-
Upset stomach and vomiting
-
Getting full very easily with only small amounts of food or drink
-
Bleeding from the rectum
-
Black, tarry stool
Online Medical Reviewer:
Marianne Fraser MSN RN
Online Medical Reviewer:
Rita Sather RN
Online Medical Reviewer:
Robyn Zercher FNP
Date Last Reviewed:
3/1/2024
© 2000-2025 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.