When Your Child Has Beta Thalassemia
Beta thalassemia is a blood disorder. It affects the production of a protein in the red blood cells (RBCs). This protein, called hemoglobin, allows RBCs to carry oxygen to all parts of the body. Hemoglobin is made up of smaller parts, including alpha globin and beta globin. When problems with beta globin lead to less hemoglobin in the blood, the condition is called beta thalassemia. Beta thalassemia can cause anemia (not enough healthy hemoglobin in the blood). Your child has been diagnosed with beta thalassemia. Your child’s healthcare provider can discuss treatment options with you.
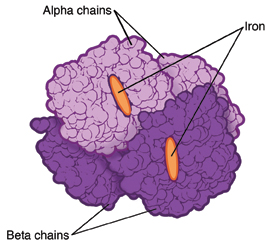 |
| Normal hemoglobin. |
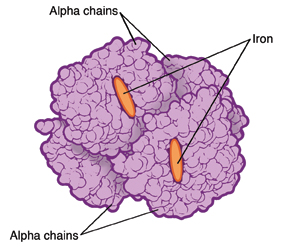 |
| Hemoglobin affected by beta thalassemia. |
Who is at risk of beta thalassemia?
This condition affects certain groups more often than others. This includes people with families from Africa and the Middle East and from Mediterranean countries such as Greece and Turkey.
What causes beta thalassemia?
Beta thalassemia is inherited. This means that the beta globin genes are passed from parent to child. There are two genes total. Problems with one or both genes can lead to different types of beta thalassemia, including:
-
Beta thalassemia minor (beta thalassemia trait). This type occurs when only one gene is affected. It may cause mild anemia.
-
Beta thalassemia intermedia. Both genes are involved. But there is some gene function. So this type is generally less severe than thalassemia major. This type is less likely to cause symptomatic anemia in early childhood that requires transfusions. But it may cause other problems, such as an enlarged spleen or liver.
-
Beta thalassemia major (Cooley’s anemia). This type can also occur when both genes are involved. It is the most severe type of beta thalassemia. It's likely to cause severe anemia that requires blood transfusions. It can also cause problems with organs such as the liver, spleen, heart, and bones.
Parents and siblings of a child with any type of beta thalassemia should be tested for the condition too. A genetic counselor can answer questions you may have.
What are the symptoms of beta thalassemia?
The symptoms of beta thalassemia depend on the type. Most children with beta thalassemia minor have few or no symptoms. Children with beta thalassemia intermedia or major may have symptoms that range from mild to severe. These may include:
-
Pale skin
-
Crankiness
-
Weakness
-
Tiredness
-
Shortness of breath
-
Trouble doing normal amounts of exercise (exercise intolerance)
-
Fast heartbeat
-
Dizziness or fainting
-
Yellowing of the eyes, skin, or mouth, and dark urine (jaundice)
-
Slowed growth
-
Weak bones
-
Stomach pain
How is beta thalassemia diagnosed?
Your child will likely see a pediatric hematologist. This is a doctor who specializes in blood disorders (hematology). The doctor will examine your child. They will ask about your child’s symptoms and health history. Tests will also be done. Most of the tests require taking a blood sample from a vein in the arm or from a finger or heel. Tests may include:
-
Complete blood cell count (CBC). This measures the amounts of types of cells in the blood.
-
Blood smear. This checks the size and shape of blood cells. A drop of blood is looked at with a microscope. A stain is added to make the parts of the blood cells easier to see.
-
Hemoglobin electrophoresis. This checks for the amounts and types of hemoglobin in the blood.
-
Other genetic or lab tests. These are done to evaluate if your child inherited the genes that can cause thalassemia.
How is beta thalassemia treated?
Most children with beta thalassemia minor need no treatment. Children with beta thalassemia intermedia or major likely need regular medical care. Treatment may include:
-
Regular doctor visits. Your child will get routine checkups and blood count tests.
-
Blood transfusions. These are done when your child’s blood cell count is too low. Most children with beta thalassemia major must have regular blood transfusions to stay healthy. As a result of frequent transfusions, iron can build up in the blood. This can cause health problems. Because of this, a treatment called chelation is also done to remove excess iron from the body.
-
Folate supplements. These help the body build more RBCs.
-
Surgery to remove the spleen or gallbladder. The spleen is an organ that stores extra blood and helps remove old RBCs from the body. Though done less often, removing the spleen may sometimes be needed. Also, surgery to remove the gallbladder may be needed if gallstones form.
-
Bone marrow transplant. In rare cases, this treatment may be done for children with severe symptoms. Diseased bone marrow cells are replaced with healthy cells from a matched donor. You’ll be told more about this treatment if it is needed.
What are the long-term concerns?
-
Beta thalassemia is a lifelong condition. Work with your child’s healthcare provider to learn how to help your child.
-
Parents who both have beta thalassemia trait can have a child with more severe disease. Talk with a genetic counselor for more information.
Coping with your child's condition
It's helpful to have support while caring for your child. Think about going to counseling. This can help you and your child deal with any worries or concerns. And get help from family, friends, community resources, or support groups. Many hospitals also have child life programs, which are designed to help children cope with illness. A hospital social worker can also answer questions and refer you to other support services, if needed. Learning more about your child’s condition and its treatments can help you feel more in control.
Online Medical Reviewer:
Adam Levy MD
Online Medical Reviewer:
Dan Brennan MD
Online Medical Reviewer:
Jessica Gotwals RN BSN MPH
Date Last Reviewed:
12/1/2022
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.