When Your Child Needs Catheter Ablation
Catheter ablation is a way to treat a heart rhythm problem (arrhythmia) in which the heart typically beats too fast (tachycardia). It's also called a tachyarrhythmia. Thin, flexible tubes (catheters) are put into veins and sometimes arteries and guided to the heart. The area of tissue that is causing the heart to beat too fast is then destroyed. This may be done with radiofrequency (RF) waves. Or it may be done with cold temperature (cryoablation). The procedure typically takes about 1 to 4 hours, but could last much longer and is done by a pediatric electrophysiologist. This is a health care provider who is trained to treat electrical problems of the heart in children.
Before the procedure
-
Tell the health care provider if your child takes medicines. Your child may need to stop taking them 3 to 5 days before the procedure.
-
Tell the provider if your child has allergies to medicines, latex, or surgical soap and what kind of reaction they had.
-
Follow the provider's instructions about what your child should not eat or drink before the procedure.
-
Follow all other instructions you are given.
During the procedure
-
You will stay in a waiting area while the procedure is done.
-
Your child is given a sedative and pain reliever through an I.V. (intravenous) line. This will help your child relax and not feel pain. Anesthesia may also be used. This is given by a face mask or I.V. A breathing tube may be placed in your child’s windpipe (trachea). Your child’s heart rate, oxygen levels, and blood pressure are watched.
-
The neck, the groin, or both are numbed with a local anesthetic. The health care provider will then put the catheters through blood vessels using I.V. lines.
-
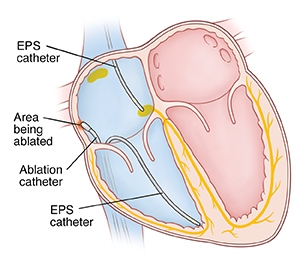
The provider will move the catheters to the inside of the heart. X-ray pictures are used to help with this.
-
An electrophysiology study is done. During this, the healthcare provider tries to start the arrhythmia. An electrical map of the inside of the heart can then be made. This shows the type of tachycardia your child has. It also shows where in the heart the abnormal area of tissue is located.
-
The provider will move an ablation catheter to that area. RF energy or cold temperature is generated at the catheter tip. This destroys the problem cells and breaks the electrical circuit causing the arrhythmia. One or more of the following may be ablated:
-
After the tissue is ablated, the provider will try again to start up the arrhythmia. If it happens again, your child may need more ablation because there may be an additional area of abnormal tissue.
-
When the procedure is done, the catheters are removed. Pressure is put on the catheter insertion sites to help them close. No stitches are needed.
After the procedure
-
Your child is taken to a recovery room. You can join your child at this time. It may take 1 to 2 hours for the anesthesia to wear off.
-
Your child will need to lie flat for 4 to 6 hours. This is how long it takes for the insertion sites to close.
-
Your child may need to stay in the hospital overnight or may go home the same day.
-
Before your child leaves the hospital, you will be given instructions for home care.
Follow-up care
Your child will need a follow-up visit. This is to review the results of the procedure. You will be told if your child can stop taking heart rhythm medicine. In many cases, one ablation is enough to treat a tachycardia. But the problem can return, or another tachycardia can develop. If this happens, your child may need a second catheter ablation or different medicine. Tell the health care provider if your child has new or returning symptoms.
Risks and possible complications of catheter ablation
Risks and possible problems include:
-
Bleeding or bruising at the catheter insertion sites.
-
Blood clot.
-
Infection.
-
A slow heart rhythm. This may need a permanent pacemaker.
-
Puncture or tearing of the heart muscle, blood vessel, or lung. This may need an emergency procedure.
-
Damage to heart valve (rare).
When should I call my child's doctor?
After the ablation procedure, call the health care provider right away if your child has:
-
A fever (see Fever and children, below).
-
Increased bleeding, bruising, warmth, redness, or pain at the catheter insertion sites.
-
Coldness, discoloration, swelling, or numbness of the arm or leg that the catheter was inserted in.
-
A bruise or lump that’s larger than a walnut at the catheter insertion sites.
-
Lightheadedness.
Call 911
Call 911 if your child has:
-
Shortness of breath or chest pain.
-
A lasting feeling that the heart is skipping or adding a beat (palpitations).
-
Fainting or isn't responsive.
-
Sudden swelling of the puncture site.
-
Bleeding from the catheter insertion site that does not slow down when you press on it firmly
Fever and children
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The health care provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use a rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any provider about your child’s fever, tell them which type you used.
Below is when to call the provider if your child has a fever. Your child’s provider may give you different numbers. Follow their instructions.
When to call a health care provider about your child’s fever
For a baby under 3 months old:
-
First, ask your child’s provider how you should take the temperature.
-
Rectal or forehead: 100.4°F (38°C) or higher
-
Armpit: 99°F (37.2°C) or higher
-
A fever of ___________as advised by the provider
For a child age 3 months to 36 months (3 years):
-
Rectal or forehead: 102°F (38.9°C) or higher
-
Ear (only for use over age 6 months): 102°F (38.9°C) or higher
-
A fever of ___________ as advised by the provider
In these cases:
-
Armpit temperature of 103°F (39.4°C) or higher in a child of any age
-
Temperature of 104°F (40°C) or higher in a child of any age
-
A fever of ___________ as advised by the provider
Online Medical Reviewer:
Stacey Wojcik MBA BSN RN
Online Medical Reviewer:
Steven Kang MD
Date Last Reviewed:
2/1/2025
© 2000-2025 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.