Understanding Lumbar Radiculopathy (Sciatica)
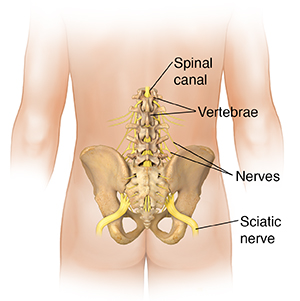
Lumbar radiculopathy is caused by irritation or inflammation of a nerve root in the lower back. It's also called sciatica. It causes symptoms that spread out from the back down to one or both legs. To understand this condition, it helps to understand the parts of the spine:
-
Vertebrae. The spine is made up of 24 small bones called vertebrae which are stacked on top of each other. The lumbar spine contains 5 vertebrae near the bottom of your spine.
-
Disks. These are soft pads of tissue between the vertebrae. They act as shock absorbers and spacers for the spine.
-
Spinal canal. This is a tunnel formed within the stacked vertebrae. Its main function is to protect the spinal cord which travels throughout the length of the spine.
-
Spinal cord. This is a long bundle of nerves that run down your back through the spinal canal in the vertebrae.
-
Spinal nerves. They branch-off the spinal canal and travel out to different parts of the body. As they leave the spinal canal, these nerves pass through openings (called foramen) between the vertebrae. The nerve root is the part of the nerve that is closest to the spinal canal.
-
Sciatic nerve. This is a large nerve formed from several nerve roots in the lower back. This nerve extends down the buttock and down the back of the leg to the foot.
With lumbar radiculopathy, nerve roots in the lower back become irritated. This leads to pain and symptoms. The sciatic nerve is commonly affected, so the condition is often called sciatica.
What causes lumbar radiculopathy?
Aging, injury, poor posture, extra body weight, and other issues can lead to problems in the lower back. These problems may then irritate nerve roots. They include:
-
Damage to a disk in the lumbar spine. The damaged disk may then press on nearby nerve roots.
-
Degeneration from wear and tear, and aging. This can lead to narrowing (stenosis) of the openings between the vertebrae. The narrowed openings press on nerve roots as they leave the spinal canal.
-
Unstable spine. This is when a vertebra slips forward. It can then press on a nerve root.
Other, less common things such as infection or a tumor can put pressure on nerves in the lower back.
Symptoms of lumbar radiculopathy
These include:
-
Shooting pain in the lower back
-
Pain, numbness, tingling, or muscle weakness that travels into the buttocks, hip, groin, or leg
-
Muscle spasms in the low back, or leg
Treatment for lumbar radiculopathy
In most cases, treatment depends on the cause and severity of symptoms. Your healthcare provider will first try treatments that help ease symptoms. These may include:
-
Prescription and over-the-counter pain medicines These help ease pain, swelling, and irritation.
-
Limits on positions and activities that increase pain. But lying in bed or avoiding all movement is only advised for a short time if necessary.
-
Physical therapy, including exercises and stretches. This helps decrease pain and increase movement and function.
-
Steroid shots into the lower back. This may help ease symptoms for a time.
-
Weight-loss. If you're overweight, losing extra pounds may help ease symptoms.
In some cases, you may need surgery to fix the underlying problem. This depends on the cause, the symptoms, and how long the pain has lasted.
In cases where symptoms don't get better, imaging studies, electromyography, and nerve conduction studies can help make a diagnosis. Severe symptoms require imaging or urgent surgery.
Possible complications
Over time, an irritated and inflamed nerve may become damaged. This may lead to long-lasting (permanent) numbness or weakness in your legs and feet. Other complications include loss of function, decreased quality of life, chronic pain and muscle shrinking. If symptoms change suddenly or get worse, tell your healthcare provider.
When to call your healthcare provider
Call your healthcare provider right away if you have any of these:
-
New pain or pain that gets worse
-
New or increasing weakness, tingling, or numbness in your leg or foot
-
Problems controlling your bladder or bowel