COPD: Chronic Coughing
When you have COPD, you may have a cough that lasts for 3 months or longer. It can last for 2 years in a row. This is called a chronic cough. A chronic cough with COPD is usually caused by irritation of the airways.
What is a chronic cough?
Coughing is a normal function of your body. It plays an important role in your breathing system. Coughing helps protect your body. It removes germs, mucus, dust, and other irritants from your lungs.
In people who don't have COPD, a cough that lasts longer than 8 weeks is also called a chronic cough. But when you have COPD, a cough can last 3 months or make a lot of mucus. Because symptoms of the condition can vary or may look like another disease, your healthcare provider will need to confirm that you have COPD.
How does COPD cause a chronic cough?
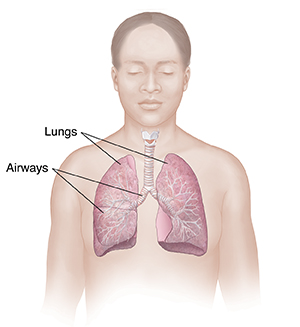
COPD is a condition that keeps your lungs from working as they should. The lungs’ job is to get air in and out of the body. Inside the lungs, air moves through tubes called airways. In healthy airways, air moves in and out easily. With COPD, some airways are blocked because of swelling to the lining of the airway and an increase in mucus. This makes breathing harder. It can also cause a chronic cough.
COPD is a term for 2 main conditions. These are chronic bronchitis and emphysema. In both of these conditions, the airways and lungs are damaged. The damage is usually from breathing in irritants over a long period of time. Irritants are particles that irritate the lungs and airways. The main irritant that causes COPD is cigarette smoke. Other irritants are pollution, dust, fumes, and chemicals. When the lungs are always irritated, the body coughs a lot. It does this to try to remove the irritants. This chronic cough is often called a smoker’s cough.
With chronic bronchitis, the damaged airways swell. They also make more mucus than normal. Mucus is a thick, sticky fluid. It traps smoke and other harmful irritants you breathe in. This helps protect the airways. However, too much mucus can block the airways, making it harder to breathe. The body tries to remove this excess mucus by coughing it up.
Treatment for chronic cough
There is no cure for COPD. But certain treatments help control a chronic cough:
-
Bronchodilators. These medicines help open the airways. This makes it easier to breathe. Most bronchodilators are taken with an inhaler or a nebulizer. This allows the medicine to go straight to the lungs.
-
Combination medicines. These include a bronchodilator and a steroid. Steroids reduce swelling and mucus production. This helps keep the airways from getting irritated. These medicines are usually taken every day to help prevent coughing and other breathing problems.
-
Antibiotics. A respiratory infection can lead to more coughing and mucus. Antibiotics are medicines that help treat bacterial infections.
-
Pulmonary rehab (rehabilitation). This program teaches ways to ease COPD symptoms. It includes tips on eating well and exercising to feel better.
-
Oxygen therapy. If your oxygen levels are low, your healthcare provider may prescribe oxygen to help make your breathing easier. Oxygen is breathed in through prongs in the nose or a facemask. Oxygen can be used only at certain times. Or it can be used most of the time.
Your healthcare provider will work with you to come up with the best treatment plan for you.
Self-care tips for chronic cough
You can take steps to reduce your coughing:
-
Stop smoking. Smoking is the main cause of COPD. Stopping smoking is the best thing you can do to treat COPD. If you need help stopping smoking, talk with your healthcare provider. There are medicines that can help you quit. There are also programs, such as the American Lung Association’s Freedom From Smoking program.
-
Stay away from secondhand smoke and other irritants. Try to stay away from smoke, chemicals, fumes, pollen, and dust. Don’t let anyone smoke in your home or around you. Stay indoors on smoggy days.
-
Prevent lung infections. Having COPD increases your risk for respiratory infections, such as the flu, pneumonia, and COVID-19. Ask your healthcare provider about the vaccines you need. Take steps to prevent colds and other lung infections. Stay away from crowds when possible during cold and flu season. Wear a mask when you are in crowded indoor places during cold and flu season.
-
Practice correct handwashing. Wash your hands often with soap and clean, running water for at least 20 seconds. Use hand sanitizer with at least 60% alcohol when you can’t wash your hands.
-
Limit dairy products. Dairy products can increase mucus. So have milk, ice cream, and cheese in small amounts.
-
Drink plenty of water. This helps make mucus thinner and easier to cough up. Ask your healthcare provider how much water you should drink. For many people, 6 to 8 glasses (8 ounces each) a day is a good goal.
-
Do breathing exercises. Learn how to do belly breathing and pursed lip breathing. These exercises can help you breathe better. Try to do each exercise for 5 to 10 minutes every day.
-
Don’t be afraid to be active. Being active may make you short of breath. Even so, it is good for your lungs. Exercise can make the muscles that help you breathe stronger. Ask your healthcare provider about safe exercises for you.
When to call your healthcare provider
Call your healthcare provider right away if you have any of these problems:
-
Fever of 100.4°F (38°C) or higher, or as directed by your healthcare provider
-
Symptoms that don’t get better, or get worse
-
New symptoms