Mastopexy (Breast Lift)
Changes in breast shape and firmness often happen due to pregnancy, weight loss, or aging. Breast tissue and skin lose their ability to expand or stretch and return to normal (elasticity). This allows the breasts to droop and lose their shape. Mastopexy is a type of cosmetic surgery done to reshape the breasts if they have sagged. It's often called a breast lift. Having a breast lift changes the look of your breasts and usually improves their appearance.
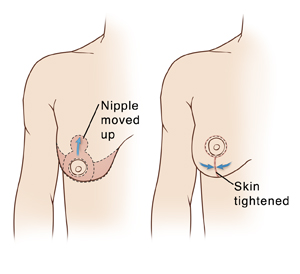 |
| This picture shows one type of mastopexy. Talk to your surgeon about how your own surgery will be done. |
Preparing for surgery
Prepare for the surgery as you have been told. In addition:
-
Tell your surgeon about all prescription and over-the-counter medicines you take. This also includes herbs and other supplements. It also includes any blood thinners, such as warfarin, certain anti-inflammatory medicines, clopidogrel, and daily aspirin. You may need to stop taking some or all of them before surgery.
-
Tell your surgeon if you think you may be pregnant or if you are ill.
-
Don't smoke or vape. Nicotine affects the blood supply of your skin and can slow wound healing. Your surgeon may choose to delay your surgery if you are smoking.
-
Follow any directions you are given for not eating or drinking before surgery. (If you have been told to take medicines, take them with a small sip of water.)
The day of surgery
The surgery takes about 2 to 4 hours. You may go home the same day. Or you may stay overnight in a hospital or outpatient surgical center.
Before the surgery begins
-
An IV (intravenous) line is put into a vein in your arm or hand. This line delivers fluids and medicines.
-
You will be given medicine to keep you pain free during surgery. This may be general anesthesia, which puts you into a state like deep sleep. (A tube may be inserted into your throat to help you breathe.) Or you may have sedation, which makes you relaxed and sleepy. If you have sedation, local anesthesia will be injected to numb the area being worked on. The anesthesiologist will discuss your choices with you.
During the surgery
-
The surgeon makes cuts (incisions) in the skin around your breast. You and your surgeon will have discussed incision sites before surgery.
-
The surgeon moves the breast tissue higher on the chest. Breast skin is tightened to hold the tissue in position. Any extra skin is removed.
-
The dark skin around the nipple (areola) and nipple are moved higher on the breast. If the size of the areola is being decreased, skin is removed. The areola is stitched into place. One of the side effects is a temporary or permanent loss of sensation in your nipples. Discuss this side effect with your surgeon before surgery.
-
The process is repeated on the other breast.
-
The incisions are closed with stitches, surgical glue, or both. A tube (drain) may be placed into an incision before it's closed. This drains excess fluid that may build up as the wound begins to heal. Staff may also put a bra on you before you wake up.
After the surgery
You will be taken to a room to the PACU (postanesthesia care unit) to be watched as you wake up from the anesthesia. You may feel sleepy and nauseated. If a breathing tube was used during surgery, your throat may be sore at first. You’ll be given medicine to control pain or nausea. When you’re ready, you will be able to go home with an adult family member or friend. Or you may be taken to a room to stay overnight.
Recovering at home
Once home, follow any directions you are given. Your surgeon will tell you when you can return to your normal routine. During your recovery:
-
Take any prescribed medicines exactly as directed.
-
Wear the special bra or bandage you were given before discharge as directed by your surgeon.
-
Care for your incisions and the dressing (bandage) over them as directed by your surgeon. Wash your hands before and after caring for your incisions and dressings.
-
Follow your surgeon’s guidelines for showering. Don't swim, take a bath, use a hot tub, or do other activities that cause the incisions to be covered with water until your surgeon says it’s OK.
-
When you shower, gently wash your incision sites. Then pat the incisions dry. Don’t apply lotions, oils, or creams to the incisions until after they are fully healed.
-
Don’t raise your arms above breast level for 10 days. And don’t lift, push, or pull anything heavier than 10 pounds for at least 7 days.
-
Don’t drive until you are no longer taking prescription pain medicine and your surgeon says it’s OK. When riding in a car, carefully position the seatbelt so that it doesn’t compress your breasts.
-
Be aware that breast swelling may last for 3 to 5 weeks. If advised by your surgeon, use a cold pack wrapped in a thin towel to relieve discomfort and control swelling. It’s important not to leave the cold pack on for too long, or your skin could be damaged. Put the pack over your bandages for no more than 20 minutes at a time. Then leave it off for at least 20 minutes. Repeat this as often as needed during waking hours until swelling starts to improve. Don’t fall asleep with the cold pack on. If you’re not sure how to safely use the cold pack, ask your surgeon.
When to call your healthcare provider
Call your surgeon or healthcare provider right away if any of the following occur:
-
Extreme chest pain or trouble breathing (call 911 )
-
A fever of 100.4° F ( 38°C ) or higher, or as directed by your healthcare provider
-
Bleeding or drainage through the special bra or bandage
-
Symptoms of infection at an incision site, such as increased redness or swelling, warmth, pain that gets worse, or foul-smelling drainage
-
Pain that is not relieved by medicine
-
More soreness, swelling, or bruising on one breast than the other
-
Breast that is very warm to the touch
Follow-up
You will have follow-up visits so your surgeon can see how well you’re healing. If needed, stitches or drains will be removed during one of these visits. If you have any questions about your recovery, let your surgeon know. Also, be aware that your breasts may sag again over time. If you have any concerns about your surgery results, talk to your surgeon.
Risks and possible complications
Risks and possible complications include:
-
Bleeding
-
Infection
-
Blood clots
-
Open wounds that take time to heal
-
Excessive or visible scarring
-
Changes in breast or nipple sensation (temporary or permanent)
-
Potential for breasts to sag again
-
Breasts that are not the same shape or size
-
Not being happy with cosmetic result
-
Risks of anesthesia
Online Medical Reviewer:
David Lickstein MD
Online Medical Reviewer:
Rita Sather RN
Online Medical Reviewer:
Tara Novick BSN MSN
Date Last Reviewed:
12/1/2022
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.