GERD (Child)
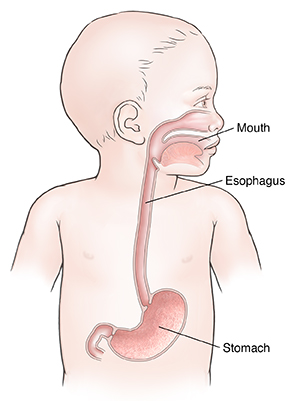
GERD stands for gastroesophageal reflux disease. You may also hear it called acid indigestion or heartburn. It happens when stomach contents flow back up (reflux) into the esophagus. The esophagus is the tube that connects the mouth to the stomach. This can irritate the esophagus. It can also cause problems with swallowing or breathing. In severe cases, GERD can cause pneumonia that keeps coming back or other serious problems.
A baby may have reflux if you see any of the following soon after eating:
Most babies show signs of some reflux during the first few weeks of life. This condition is often harmless. By 7 months, the valve in the esophagus should be more developed, and symptoms should ease. By the time a baby has been walking for 3 months, reflux normally has gone away.
Symptoms of GERD in older children include:
-
Food or liquid coming up in the back of the mouth (spitting up)
-
Feeling of burning in the chest (heartburn) or stomach pain
-
Belching
-
Bad breath
-
Acid or bitter taste in the mouth
-
Cough that continues, especially at night or on waking
Home care
For children younger than age 2:
-
Burp your baby several times during and after feeding.
-
Don't feed your baby lying down.
-
Don't overfeed. Wait at least 2 to 3 hours between feedings so the stomach can empty. Or give smaller amounts more often.
-
Keep your baby in an upright position during feeding and for 20 to 30 minutes after each feeding. Do this by carrying your baby in an upright position. For example, over your shoulder. Don't place your baby in a baby carrier or car seat.
-
Don't use tight diapers. They will put pressure on the belly (abdomen).
-
Place your baby on their back to sleep. Never put your baby to sleep on their stomach. Babies younger than age 1 should be placed on their backs to sleep. Do this even if they have reflux. Placing babies younger than age 12 months on their stomachs or sides can increase the risk for SIDS (sudden infant death syndrome).
For children age 2 and older:
-
Don't feed within 2 to 3 hours before bedtime.
-
Keep the chest higher than the stomach during sleep. You can do this by placing 2- to 4-inch blocks under the head of the bed or crib. Or you can use extra pillows under the head and shoulders.
-
If your child is overweight, talk with your child's healthcare provider about making a plan to help your child lose weight. Being overweight makes GERD more likely.
-
Have your child wear clothes with a looser waistband.
-
Ask your child's provider whether to limit any foods or drinks. These may include fatty or spicy foods.
Medicines
The lifestyle changes above may be enough to manage a child's GERD. But your child may need medicine in some cases. If medicines may help your child, your child's healthcare provider will discuss a treatment plan with you. Don't give any medicines to your child without talking with your child's provider first. Children should not take medicines for GERD without a provider's supervision.
Follow-up care
Follow up with your child's healthcare provider, or as advised.
When to seek medical advice
Call your child's healthcare provider right away if any of the following occur:
-
Severe coughing spell, trouble breathing, or wheezing
-
Fast breathing
-
Repeated vomiting
-
Blood in the stool (red or black color) or vomit
-
Belly or chest pain that gets worse
-
Symptoms get worse or your child has new symptoms
Call 911
Call 911 if your child has trouble breathing or swallowing.