COPD Flare-Up
You have had a flare-up of your COPD.
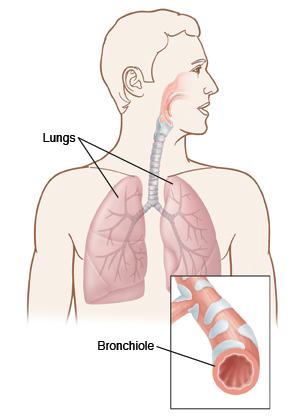
COPD (chronic obstructive pulmonary disease) is a common lung disease. It causes your airways to get irritated and narrower. This makes it harder for you to breathe. Emphysema and chronic bronchitis are both types of COPD. This is a long-term (chronic) condition. This means you always have it. Sometimes it gets worse. When this happens, it's called a flare-up.
Symptoms of COPD
People with COPD may have symptoms most of the time. In a flare-up, your symptoms get worse. These symptoms may mean you are having a flare-up:
-
Shortness of breath, shallow or rapid breathing, or wheezing that gets worse
-
Lung infection
-
Cough that gets worse
-
More mucus (or sputum), thicker mucus, or mucus of a different color
-
Tiredness, less energy, or trouble doing your normal activities
-
Fever
-
Chest tightness
-
Your symptoms don’t get better even when you use your normal medicines, inhalers, and nebulizer
-
Trouble talking
-
You feel confused
Causes of flare-ups
Unfortunately, a flare-up can happen even if you did everything right, and even if you followed your healthcare provider’s instructions. Some causes of flare-ups are:
-
Cold weather
-
Smoking or secondhand smoke
-
Use of e-cigarettes or vaping products
-
Colds, the flu, or respiratory infections
-
Air pollution
-
Sudden change in the weather
-
Dust, vapors, gases, irritating chemicals, or strong fumes
-
Not taking your medicines as prescribed
-
Indoor pollution such as burning wood, smoke from home cooking, or heating fuels
Home care
Here are some things you can do at home to treat a flare-up:
-
Keep calm and try not to panic. This makes it harder to breathe, and keeps you from doing the right things.
-
Don’t smoke or be around others who are smoking. If you smoke, quit. Smoking is the main cause of COPD. Quitting will help you be able to better manage your COPD. Don't use e-cigarettes or vaping products either. Ask your healthcare provider about ways to help you quit smoking.
-
Before drinking extra fluids during flare-ups to loosen the mucus, always talk with your healthcare provider first.
-
Eat a healthy, balanced diet. This is important to staying as healthy as possible. So is trying to stay at your ideal weight. Being overweight or underweight can affect your health. Make sure you have a lot of fruits and vegetables every day. And also eat balanced portions of whole grains, lean meats and fish, and low-fat dairy products.
-
Use your inhalers and nebulizer, if you have one, as you have been told to. When using a metered dose inhaler or nebulizer, it's very important to use the proper techniques. If you have any questions about how to use your device, contact your healthcare provider or refer to the user manual.
-
If you were given antibiotics, take them until they are used up or your provider tells you to stop. It’s important to finish the antibiotics even though you feel better. This will make sure the infection has cleared.
-
If you were given a steroid, finish it even if you feel better.
-
Learn the names of your medicines, as well as how and when to use them. Talk with your provider about other conditions you have and their treatment and how it may affect your COPD.
-
Oxygen may be prescribed if tests show that your blood contains too little oxygen. Ask your provider about long-term oxygen therapy.
-
Coping tips for shortness of breath include:
-
Exercise. Try to be as active as possible. This will improve energy levels and strengthen your muscles so you can do more.
-
Breathing methods. Ask your healthcare provider or nurse to show you how to do pursed-lip breathing.
-
Balance rest and activity. Each day, try to balance rest periods with activity. For example, you might start the day with getting dressed and eating breakfast. Then you can relax and read the paper. After that, take a brief walk. And then sit with your feet up for a while.
-
Pulmonary rehab (rehabilitation). Community-based and home-based programs work as well as hospital-based programs as long as they are as often and as intense. Standard home-based pulmonary rehab programs help shortness of breath in people with COPD. Supervised, traditional pulmonary rehab remains the best option for people with COPD. These programs help with managing your disease and also help with breathing methods, exercise, support, and counseling. To find one, ask your provider or call your local hospital. Also talk with your healthcare provider about which rehab or self-management program is best for you.
Preventing a flare-up
Flare-ups happen. But the best way to treat one is to prevent it before it starts. Here are some pointers:
-
Don’t smoke or be around others who are smoking. Avoid using e-cigarettes due to their harmful side effects.
-
Take your medicines as discussed with your healthcare provider.
-
Talk with your provider about getting a flu shot every year. Also find out if you need a pneumonia shot.
-
If there is a weather advisory warning to stay indoors, try to stay inside when possible.
-
Try to eat healthy, exercise, and get plenty of sleep.
-
Try to stay away from things that normally set you off. These include dust, chemical fumes, hairsprays, or strong perfumes.
Follow-up care
Follow up with your healthcare provider as advised.
If a culture was done, you will be told if your treatment needs to be changed. You can call as directed for the results.
If X-rays were done, you will be told of any new findings that may affect your care.
During each appointment, talk with your healthcare provider about your ability to:
-
Cope in your normal environment
-
Correctly use inhaler (or your medicine delivery systems)
-
Cope with other conditions you have and their treatments and how they may affect your COPD
Call 911
Call 911 if any of these occur:
-
Wheezing or shortness of breath does not get better with treatment
-
Chest pain or chest tightness
-
Feeling lightheaded or dizzy
-
You have trouble breathing
-
You feel confused or it’s hard to wake you up
-
You faint or lose consciousness
-
You have a rapid heart rate
-
You have new pain in your chest, arm, shoulder, neck, or upper back
When to seek medical advice
Call your healthcare provider right away if any of these occur:
-
Fever of 100.4°F (38ºC) or higher, or as directed by your healthcare provider
-
Coughing up lots of dark-colored or bloody mucus (sputum)
-
You don't start to get better within 24 hours or new symptoms develop
-
Swelling of your ankles gets worse
-
Weakness
Online Medical Reviewer:
Daphne Pierce-Smith RN MSN
Online Medical Reviewer:
David A Kaufman MD
Online Medical Reviewer:
Pat F Bass MD MPH
Date Last Reviewed:
1/1/2022
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.