Understanding Thoracic Epidural Injection
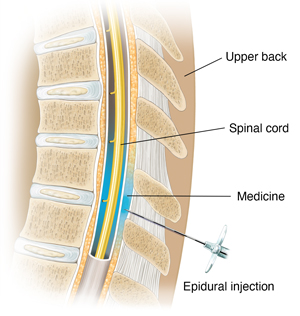
A thoracic epidural injection is a shot that helps ease pain in your upper to middle back (thoracic) area. Medicine is injected into the area around your spinal cord.
About the spinal cord
Your spinal cord is a bundle of nerves that runs from the base of your brain to your lower back. The spinal nerves run off either side of it. Your spinal cord is surrounded and protected by your backbone (spine). It's made up of many small bones stacked on top of each other (vertebrae). Cushions (intervertebral disks) are between the vertebrae. The space between the covering of the spinal cord (dura) and the spine is the epidural space.
Why a thoracic epidural injection is done
A spinal nerve can become pinched or inflamed. That may happen if a disk presses on a nerve. This can happen anywhere along your spinal cord and spine. It may cause pain in the area. The pain may also extend to other areas of your body.
A thoracic epidural injection may give pain relief for problems that affect the thoracic spine such as:
-
Part of a disk squeezing against a nerve (disk herniation)
-
Narrowing in the space for the nerve (spinal stenosis)
-
Long-term pain after back surgery (post-surgery spine syndrome)
-
An injury that irritates a spinal nerve
A thoracic epidural injection may be done if other treatments don’t work to ease your pain. The injection may help ease pain in your middle to upper back for weeks to months or longer. You may have more than one injection, but not usually more than one in a month.
An epidural injection may also be used to help diagnose the source of your pain. Your healthcare provider will inject numbing medicine (local anesthetic) into the epidural space. If your pain quickly goes away, your healthcare provider will know that a nerve is causing your pain. They can then treat your pain better.
How thoracic epidural injection is done
A pain specialist, radiologist, neurosurgeon, orthopedic surgeon, or other type of specialist may do the procedure. You will lie on your belly (abdomen) or on your side on a special table. Your healthcare provider will use special imaging tools with either X-ray (fluoroscopy) or CT scan to put the needle into the correct area. They will inject contrast dye to make sure the needle is in the epidural space. They will slowly inject medicine. It's usually a mix of anti-inflammatory medicine (steroid) and numbing medicine (anesthetic). The steroid medicine lessens swelling and nerve irritation. The anesthetic medicine numbs the area. You may feel slight discomfort and pressure when the medicine is injected. This usually disappears once all of the medicine is injected.
Risks of thoracic epidural injection
Most procedures have some risks. The risks of this procedure include:
Your own risks may differ. They depend on your age, overall health, and other factors. You may not be able to have an injection if you have a health condition such as:
-
Infection
-
Bleeding disorder
-
Uncontrolled high blood pressure
-
Diabetes
-
Heart-related chest pain (unstable angina)
-
Heart failure
-
Allergy to contrast dye, local anesthetics, or steroids
Talk with your healthcare provider about your specific risks.
Online Medical Reviewer:
Callie Tayrien RN MSN
Online Medical Reviewer:
Jimmy Moe MD
Online Medical Reviewer:
Tara Novick BSN MSN
Date Last Reviewed:
12/1/2022
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.