Diabetes and Your Child: Understanding Type 1 Diabetes
You’ve been told that your child has type 1 diabetes. This means their pancreas can't make insulin. In type 1 diabetes, an autoimmune disorder causes the body to destroy the cells in the pancreas that make insulin. Without enough insulin, blood sugar can't enter the cells to be used for energy. So, it builds up in the blood (hyperglycemia). Diabetes is a lifelong condition. Left untreated, it can lead to serious health problems. But diabetes can be managed with correct treatment and lifestyle changes. This lets your child live a full, healthy life.
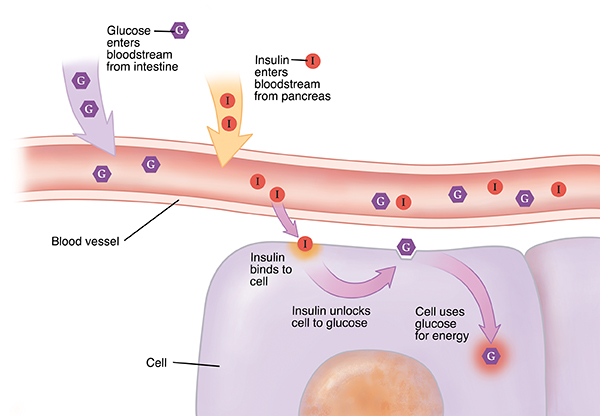
How the body gets energy
When your child eats, the digestive system breaks down food. Some of this food is turned into glucose in the intestine. Glucose (also called blood sugar) gives energy to the body’s cells. It travels through the blood to reach the cells. But glucose needs the help of a hormone called insulin to enter cells. Insulin is made by the pancreas. Insulin is released into the blood. It travels to the cells just like glucose. When insulin reaches a cell, it acts like a key. It opens a door into the cell so glucose can enter.
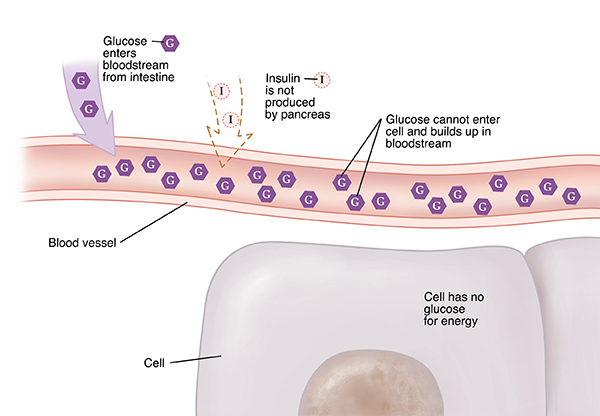
When your child has type 1 diabetes
In children with type 1 diabetes, the pancreas stops making insulin. Food is still broken down into glucose. And glucose still travels to the cells. But without insulin, glucose can’t enter the cells. Instead, it builds up in the blood. The liver puts more glucose out into the blood. Too much glucose in the blood is called hyperglycemia (high blood sugar). Without glucose, your child’s cells don’t get the energy they need. And over time, high blood sugar can cause other health problems.
What are the causes of type 1 diabetes?
The exact cause of type 1 diabetes isn't known. It occurs when the body's immune system starts targeting the insulin-producing cells in the pancreas. We do know that it’s not caused by eating too much sugar. Type 1 diabetes can run in families. Or your child may be the only person in the family to have type 1 diabetes. The important thing to remember is that it’s not your fault. Nothing you or your child did caused their diabetes. Having certain genes or being exposed to certain viruses may cause type 1 diabetes.
A new medicine was approved to help delay the onset of type 1 diabetes. This may be a choice for people ages 8 and older who are at high risk or have early signs of type 1 diabetes.
What are the symptoms of type 1 diabetes?
When the pancreas stops making insulin or makes very little insulin, the body’s cells become starved for energy. This can make your child feel tired and rundown. Your child may feel or have:
-
Very strong thirst.
-
Increased peeing.
-
Blurry vision.
-
Tired for no clear reason.
-
Extreme hunger.
-
Headaches.
-
Flu-like symptoms.
-
Bed wetting.
-
Unexplained weight loss.
-
Trouble focusing.
-
Upset stomach (nausea), vomiting, and belly pain.
How is type 1 diabetes diagnosed?
Simple blood tests can help the doctor find out if your child has type 1 diabetes. These tests check for a high level of glucose in your child’s blood. Glucose tests may need to be repeated to confirm the diagnosis.
Your child's doctor may order other tests as well to confirm the diagnosis. These tests include levels of a substance called C-peptide and certain antibodies in the blood.
Autoantibody-based screening for type 1 diabetes before any symptoms show should be offered to those with a family history of type 1 diabetes.
How is type 1 diabetes treated?
There's no cure for type 1 diabetes. But it can be managed. Your child’s pancreas isn't making enough insulin. So insulin has to be put into your child’s body. Insulin is most often given as a shot. The idea of giving your child shots might seem scary at first. But most parents and children find that it’s easier than they thought. Insulin pens are accurate, easy to use and practically pain-free, even for children. Your child may be able to use an insulin pump that helps give insulin. Your child’s doctor will teach you how to check your child’s blood sugar level. This tells you how much insulin to give your child to keep blood sugar in a healthy range. Your child may be able to use a continuous glucose monitor to check their blood sugar level.
What are the long-term concerns?
People with a blood sugar level that's too high over many years can develop health problems. These problems can affect the heart, eyes, kidneys, and nerves. You can help delay or prevent these problems in your child. To do this, manage your child’s blood sugar as directed. Support and role model a healthy lifestyle. And teach your child in an age appropriate way how to manage their diabetes. Also, be aware of the symptoms of low blood sugar levels (hypoglycemia). These symptoms include headache, confusion, slurred speech, sweating, and irritable mood. Learn what to do when your child has low blood sugar. Teach other caregivers (such as those at your child's school or daycare) the same so that they may help in an emergency. Have your child wear a medical ID that says they have diabetes and whom to contact in case of an emergency.
The honeymoon phase
After diagnosis, your child’s pancreas may still be making a little insulin on its own. This is called the honeymoon phase. At this time, your child’s blood sugar may be managed with very little insulin. The honeymoon phase may last months or even years. Because of this, you may think that your child’s diabetes has gone away or been cured. But this isn't the case. As time goes on, your child’s pancreas will stop being able to make any insulin at all. Talk to your child’s doctor about managing your child’s blood sugar during the honeymoon phase.
Note
This sheet doesn't give all the information you need to care for your child with diabetes. Ask your child’s doctor for more information.
To learn more
For more information about diabetes, visit these websites:
How daily issues affect your health
Many things in your daily life impact your health. This can include transportation, money problems, housing, access to food, and child care. If you can’t get to medical appointments, you may not receive the care you need. When money is tight, it may be difficult to pay for medicines. And living far from a grocery store can make it hard to buy healthy food.
If you have concerns in any of these or other areas, talk with your care team. They may know of local resources to assist you. Or they may have a staff person who can help.