When Your Child Has Hypertrophic Cardiomyopathy
Hypertrophic cardiomyopathy is a problem with the heart muscle. It may not cause symptoms that bother your child. But it can lead to serious problems over time. It can usually be managed. Your child’s healthcare provider will talk with you about treatment choices. This sheet tells you more about this problem and how it's treated.
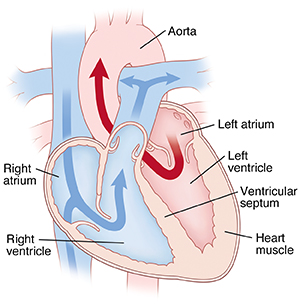
The normal heart
The heart is divided into four chambers that hold blood as it moves through the heart. The two upper chambers are called atria. The two lower chambers are called ventricles. The heart has four valves between the chambers. The valves open and close to keep blood flowing through the heart.
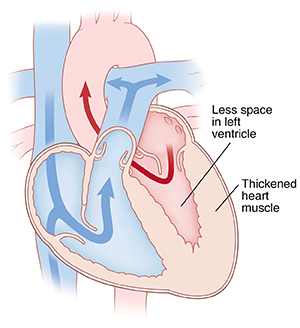
What is hypertrophic cardiomyopathy?
With this condition, the heart muscle thickens. Heart muscle that's too thick can’t pump blood normally. It may affect both ventricles. Or it may affect only one, most often the left ventricle. In some cases, it may just affect the wall that separates the ventricles. This is called the ventricular septum.
Why is hypertrophic cardiomyopathy a problem?
A thickened heart muscle can:
-
Impair blood flow leaving the heart. The thickened wall can block the flow of blood from the heart to the body. Or it can force the valves to close too soon due to changes in pressure. This forces the heart to work harder than normal to pump blood. If the heart no longer pumps blood well, a condition called heart failure can develop. With heart failure, the inability of the heart to pump blood well can cause a backup of blood and fluid in your lungs, abdomen, liver, and limbs. This can weaken the heart muscle more. Over time other organs in the body will suffer from not enough blood flow.
-
Damage heart valves. The mitral valve is most likely to be affected. This valve is between the left atrium and the left ventricle. Blood may leak backward through the valve. This is called valve insufficiency. Excess blood leaking through the valve puts strain on the ventricle. It has to pump extra hard to get all the blood out.
-
Damage electrical cells in the heart. The thickened heart can change the way electricity is conducted through the heart. This can affect the cells that control the beating of the heart. Damage to these cells can cause abnormal heart rhythms (arrhythmias). In rare cases, a severe arrhythmia can lead to sudden death.
What causes hypertrophic cardiomyopathy?
This condition can occur in your child by chance. A cause may not always be found. But it's one of the most common inherited (genetic) diseases of the heart muscle. It may be passed from a parent to child in some families. If you or your child has this condition, each close family member should be tested for it. It's important to let your healthcare provider know if there is a history of sudden cardiac death in the family or death at a young age.
What are the symptoms of hypertrophic cardiomyopathy?
Most children with this condition have no symptoms. If they do occur, they often show up when children are active. Symptoms may include:
-
Lightheadedness, dizzy spells, or fainting
-
Rapid, pounding heartbeat
-
Shortness of breath or tiredness
-
Tightness or pressure in the chest
-
Fatigue or having little energy for usual activities
How is hypertrophic cardiomyopathy diagnosed?
Heart problems in children are managed by a pediatric cardiologist. The pediatric cardiologist will give your child a physical exam to check for a heart problem. Your child may have tests to help confirm a diagnosis or tell more about the heart problem. These tests may include:
-
Echocardiogram. Sound waves (ultrasound) are used to make a picture of the heart. This helps find problems with heart structure or function.
-
Electrocardiogram. This test records the electrical activity of the heart. It helps find arrhythmias or some problems with heart size or structure.
-
Holter or event monitor. This test records the electrical activity of the heart over time. It's done with a device worn from a few days to a few weeks. It can help find problems with the heart rhythm.
-
Exercise stress test. This records the electrical activity of the heart while your child exercises. It helps find problems with the heart that may show up when the heart beats faster.
-
Cardiac MRI. This test uses a strong magnet to create detailed images of the heart and the heart muscle.
How is hypertrophic cardiomyopathy treated?
Treatment is aimed to reduce symptoms and help prevent heart failure. It can help reduce the risk of severe arrhythmia and sudden death. Your child’s treatment plan may include:
-
Medicines. Beta-blockers and calcium channel blockers may be prescribed. These medicines can lower blood pressure and slow heart rate. They help to prevent arrhythmias. They may improve the heart’s pumping action.
-
Surgery. This is done in severe cases. Surgery removes a piece of the heart muscle that is abnormally thickened. This is called a myectomy. Surgery is done when the blood flow out of the heart is blocked from the thickened muscle. Surgery improves blood flow from the heart to the body.
-
Alcohol septal ablation. This procedure is not surgery. During the ablation, the healthcare provider injects alcohol into a heart artery. This scars overly thickened heart muscle to help with blood flow. It is rarely done in children. But it may be an option.
-
Implantable cardioverter defibrillator (ICD). In some cases, hypertrophic cardiomyopathy raises the risk of a dangerous arrhythmia. An ICD is a device that is placed in the chest. It tracks the heart rate. When needed, it delivers an electric shock to the heart. This is done to stop a life-threatening heart rhythm.
-
Heart transplant. In rare cases, a heart transplant may be needed. Your child’s cardiologist will discuss this with you.
How shared decision-making can help
Testing and treatment for this heart condition can vary. What might be the right choice for one child may not be a good choice for another. The American College of Cardiology advises shared decision-making for children with or at risk for hypertrophic cardiomyopathy.
Shared decision-making is when patients, caregivers, and healthcare providers work together to make care decisions. This improves health outcomes. It can help you work with your child's care team to personalize your decisions and find the right choice for your child.
Shared decision-making includes:
-
Talking about all testing and treatment choices
-
Their risks, benefits, and expected outcomes
-
The child's and family's own values, goals, and preferences
What are long-term concerns?
-
With treatment, most children with this condition can be active. But they may have to limit certain sports or physical activities. Talk with your child's healthcare provider about activities that are safe for your child.
-
Your child needs to have regular visits with the cardiologist for the rest of their life. This is to check that their heart is working correctly. If an ICD is placed, this needs regular checks.
-
Your child may need to take medicine for the rest of their life.
When should I call my child's healthcare provider?
Contact your child's provider if your child has any of these: