Your Child Has Crohn's Disease
Crohn’s disease is a type of inflammatory bowel disease (IBD). It causes swelling, inflammation, and sores in your child’s digestive tract. The whole tract may be affected, from the mouth to the anus (where stool leaves the body). But it most often affects the end of the small bowel and beginning of the colon. Swelling, inflammation, and sores make it harder for the body to get nutrients from food. This can make your child feel very ill. It can also lead to problems with growth. No one knows what causes Crohn’s disease. There is no known cure. But your child’s symptoms can be managed.
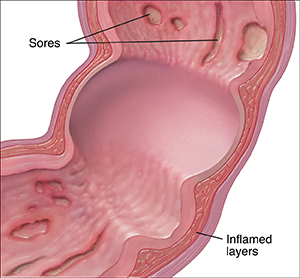 |
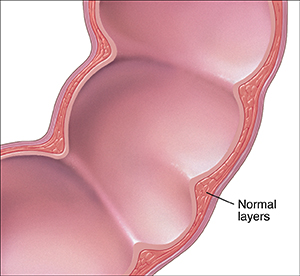
| All layers of the digestive tract can become inflamed, even the inner lining and outer walls. |
What are the symptoms of Crohn’s disease?
Common symptoms of Crohn’s disease include:
-
Belly pain
-
Fever
-
Diarrhea
-
Urgent need to move bowels
-
Growth failure (short stature)
-
Nausea or vomiting
-
Weight loss
-
Severe tiredness (fatigue)
-
Sores in the mouth or around the anus
-
Bleeding from the rectum (where stool collects before leaving the body)
-
Abscess (infection) or fistula (abnormal opening in the digestive tract)
How is Crohn’s disease diagnosed?
The healthcare provider will start by examining your child and asking some questions. Your child may also need certain tests, such as:
-
Upper GI series with small bowel follow-through. This is a series of X-rays of your child’s upper digestive tract and small intestine.
-
Blood and stool tests.
-
CT scan or MRI. These tests take detailed pictures from outside your child’s body.
-
Endoscopy and colonoscopy. During these tests, a flexible tube with a camera is used to view the inside of your child's digestive tract. This allows the healthcare provider to take a tiny tissue sample (biopsy) that will be examined at a lab.
-
Wireless capsule endoscopy. Your child swallows this small wireless camera like a pill. The camera takes pictures of the inside of the intestine. It comes out in the stool with a bowel movement. Pictures are uploaded to a computer to be analyzed.
How is Crohn’s disease treated?
Your child will be referred to a pediatric gastroenterologist. This is a healthcare provider who is an expert in managing Crohn's disease and other digestive tract problems. There is no known cure for Crohn’s disease. But there are ways to help your child feel better. These may include:
-
Medicines. These control swelling, inflammation, and sores. They may be taken by mouth or injected.
-
Supplements. These give extra nutrition.
-
Change in diet. This includes a bland (less spicy) diet, low-residue diet, lactose-free diet, or other changes depending on your child's disease and complications.
-
Bowel rest. This gives the intestines time to recover. If your child’s symptoms have been severe, the healthcare provider may suggest giving your child TPN (total parenteral nutrition). During TPN, nutrients are given through a vein in the arm or chest. This gives your child nutrition without going through the digestive tract.
-
Surgery. This may relieve your child’s symptoms. Taking medicine may not be enough to prevent flare-ups. In this case, the healthcare provider may talk to you about a surgery to help control symptoms.
Following up with the healthcare provider
Once symptoms are under control or "quiet" (in remission), the gastroenterologist will want to see your child 3 to 4 times a year for follow-up. Your child's primary healthcare provider and gastroenterologist will work together to see that your child's vaccines are up to date. They'll also watch your child's growth and well-being. Tests may be done, such as:
Handling flare-ups
Flare-ups are times when your child feels symptoms. These may still happen. These tips can help you and your child deal with flare-ups:
-
Allow more time for your child to get ready in the morning. During a flare-up, your child may need longer bathroom time. Stress and pressure can make symptoms worse. Make sure your child has plenty of time and doesn’t feel rushed.
-
Talk to your child’s teachers and school officials about your child’s Crohn’s disease. Talk with your child’s teachers about flare-ups. Ask them to let your child use the bathroom as needed. This can help prevent accidents. Also, children with Crohn’s may miss school more often during flare-ups. Work with your child’s teachers to help your child keep up with schoolwork. Your child should qualify for school accommodations under Section 504 of the Rehabilitation Act of 1973. Your healthcare provider can assist your child in getting these accommodations by writing a letter to the school.
-
Let your child be active. Having Crohn’s disease doesn’t mean your child can’t play sports or be active. During flare-ups, your child might not feel well enough to be active. Let your child decide how much activity feels OK during flare-ups. Encourage your child to be active when symptoms are quiet.
-
Encourage good nutrition. A healthy diet provides good nutrition for growth. Talk to your child about making healthy food choices when away from home.
-
Make sure your child takes all of their medicines. This can help reduce the number of flare-ups.
-
Look into Crohn’s disease support groups and resources. If your child is feeling alone or different from peers, a support group can offer tips on helping your child lead a normal, active life.
Learn more about living well with Crohn’s disease
Check out these resources:
Online Medical Reviewer:
L Renee Watson MSN RN
Online Medical Reviewer:
Liora C Adler MD
Online Medical Reviewer:
Rita Sather RN
Date Last Reviewed:
6/1/2022
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.