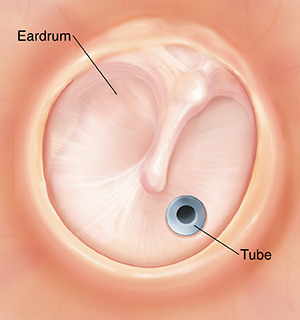
Tympanostomy (Ear Tube)
Tympanostomy is a type of ear surgery. It puts a tiny tube into the eardrum. The tube drains fluid buildup and balances air pressure on both sides of the eardrum. This procedure may be used to treat chronic ear infections or fluid buildup that reduces hearing.
Before the procedure
-
Unless you’re told otherwise, stop giving your child food and drink at least 4 hours before the scheduled arrival time. Check the exact time with the surgeon's office.
-
Your child will have a physical exam. Their temperature will be taken to rule out any active infection. This could require postponing surgery.
-
When you arrive, your child may be given medicine (a mild sedative) to help them relax.
-
You—as parent or legal guardian—will be given a consent form to sign after the healthcare provider has talked with you about the procedure. Make certain all of your questions are answered before you sign the form.
During the procedure
-
Your child will likely get general anesthesia. They will be asleep and won't feel pain during the surgery.
-
Using an operating microscope and special tools, the surgeon will make a small slit in the eardrum (tympanotomy).
-
The surgeon will use a suction tube to gently remove fluid buildup through the slit in the eardrum. In some cases, a fluid sample may be sent to a lab to see if the infection is still active.
-
The surgeon will put a tiny tube into the same slit in the eardrum (tympanostomy). Once in position, the shape of the tube helps keep it in place. Tubes can be made of plastic or metal. They vary slightly in size and shape.
After the procedure
-
Within a half-hour, your child will wake up. When you join your child, don’t be alarmed if they are upset. Anesthesia may reduce self-control. This causes some children to cry or scream.
-
Once your child is calm enough to sit up and drink fluids, they can go home.
-
At home, be sure to give your child any ear drops or other medicine as directed by the healthcare provider.
-
Go to all follow-up appointments as scheduled.
When to call your child's healthcare provider
Call your child's healthcare provider if your child has any of these signs or symptoms:
-
The ear bleeds heavily or keeps bleeding after the first 48 hours.
-
Sticky or discolored fluid drains out of the ear after the first 48 hours.
-
Your child has a fever (see Fever and children, below).
-
Your child has had a seizure caused by the fever.
-
You child is dizzy, confused, extremely drowsy, or has a change in mental state.
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds of digital thermometers. They include ones for the mouth, ear, forehead (temporal), rectum, or armpit. Ear temperatures aren’t accurate before 6 months of age. Don’t take an oral temperature until your child is at least 4 years old.
Use a rectal thermometer with care. It may accidentally poke a hole in the rectum. It may pass on germs from the stool. Follow the product maker’s directions for correct use. If you don’t feel OK using a rectal thermometer, use another type. When you talk to your child’s healthcare provider, tell them which type you used.
Below are guidelines to know if your child has a fever. Your child’s healthcare provider may give you different numbers for your child.
A baby under 3 months old:
A child age 3 months to 36 months (3 years):
-
Rectal, forehead, or ear: 102°F (38.9°C) or higher
-
Armpit: 101°F (38.3°C) or higher
Call the healthcare provider in these cases:
-
Repeated temperature of 104°F (40°C) or higher
-
Fever that lasts more than 24 hours in a child under age 2
-
Fever that lasts for 3 days in a child age 2 or older
Online Medical Reviewer:
Ashutosh Kacker MD
Online Medical Reviewer:
Marianne Fraser MSN RN
Online Medical Reviewer:
Tara Novick BSN MSN
Date Last Reviewed:
6/1/2022
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.