Understanding Middle Ear Infections in Children
Middle ear infections are most common in children under age 5. Crankiness, a fever, and tugging at or rubbing the ear may all be signs that your child has a middle ear infection. This is especially true if your child has a cold or other viral illness. It's important to call your healthcare provider if you notice any of these symptoms of a middle ear infection, or the signs listed below.
What are middle ear infections?
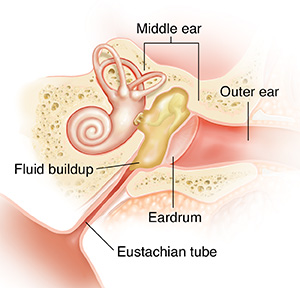
Middle ear infections occur behind the eardrum. The eardrum is the thin sheet of tissue that passes sound waves between the outer and middle ear. These infections are usually caused by bacteria or viruses. These are often related to a recent cold or allergy problem.
It's important to stop smoking in the home or around children to help prevent ear infections. Keep your child away from secondhand smoke too.
A blocked tube
In young children, these bacteria or viruses likely reach the middle ear by traveling the short length of the eustachian tube from the back of the nose. Once in the middle ear, they multiply and spread. This irritates delicate tissues lining the middle ear and eustachian tube. If the tube lining swells enough to block off the tube, air pressure drops in the middle ear. This pulls the eardrum inward, making it stiffer and less able to transmit sound.
Fluid buildup causes pain
Once the eustachian tube swells shut, moisture can’t drain from the middle ear. Fluid that should flush out the infection builds up in the chamber. This may raise pressure behind the eardrum and increase pain. But if the infection spreads to this fluid, pressure behind the eardrum goes way up. The eardrum is forced outward. It becomes painful and may break.
Chronic fluid affects hearing
If the eardrum doesn’t break and the tube remains blocked, the fluid becomes an ongoing (chronic) condition. As the immediate (acute) infection passes, the middle ear fluid thickens. It becomes sticky and takes up less space. Pressure drops in the middle ear once more. Inward suction stiffens the eardrum. This affects hearing. If the fluid is not removed, the eardrum may be stretched and damaged.
Signs of middle ear infection
-
A fever over 100.4° F ( 38.0°C) and cold symptoms
-
Severe ear pain
-
Any kind of discharge from the ear
-
Ear pain that gets worse or doesn’t go away after a few days
When to call your child's healthcare provider
Call your child's healthcare provider's office if your otherwise healthy child has any of the signs or symptoms described below:
-
Fever of 100.4°F (38°C) or higher, or as directed by your provider (see Fever and children, below)
-
Trouble swallowing
-
Your child acts ill after the fever is gone
-
Persistent brown, green, or bloody mucus
-
Signs of dehydration. These include severe thirst, dark yellow urine, infrequent urination, dull or sunken eyes, dry skin, and dry or cracked lips.
-
Your child still doesn't look or act right to you, even after taking a nonaspirin pain reliever
Call 911
Call 911 if your child has any of the following;
-
A seizure caused by the fever
-
Rapid breathing or shortness of breath
-
A stiff neck or severe, persistent headache
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use a rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below is when to call the healthcare provider if your child has a fever. Your child’s healthcare provider may give you different numbers. Follow their instructions.
When to call a healthcare provider about your child’s fever
For a baby under 3 months old:
-
First, ask your child’s healthcare provider how you should take the temperature.
-
Rectal or forehead: 100.4°F (38°C) or higher
-
Armpit: 99°F (37.2°C) or higher
-
A fever of ___________as advised by the provider
For a child age 3 months to 36 months (3 years):
-
Rectal or forehead: 102°F (38.9°C) or higher
-
Ear (only for use over age 6 months): 102°F (38.9°C) or higher
-
A fever of ___________ as advised by the provider
In these cases:
-
Armpit temperature of 103°F (39.4°C) or higher in a child of any age
-
Temperature of 104°F (40°C) or higher in a child of any age
-
A fever of ___________ as advised by the provider