Understanding Reactive Airways Dysfunction Syndrome (RADS)
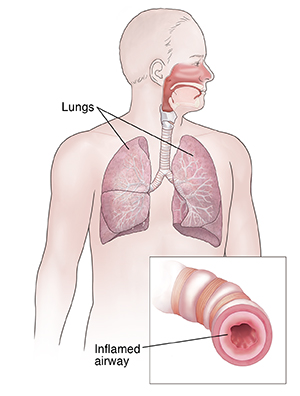
Reactive airways dysfunction syndrome (RADS) is an asthma-like condition. RADS can occur after a single exposure to very high levels of an irritant. Or it can happen after repeated exposures to low or moderate levels of an irritant. An irritant is a substance that causes swelling, tightening (narrowing), or other harmful effects of the airways in the lungs. This makes it hard to breathe. An irritant may be a chemical, dust, gas, smoke, fumes, or vapor. RADS can occur after you breathe in an irritant at home, at work, or in the environment.
RADS is not an allergic reaction. People with RADS typically have no past history of asthma or other lung diseases. But RADS can become a long-term (chronic) condition. If that occurs, your quality of life may be affected.
Symptoms of RADS
Symptoms occur right away or within 24 hours after you are exposed to the irritant. RADS symptoms are very much like asthma symptoms. They can be mild or severe. Symptoms may include:
Symptoms may last up to 1 year. They often respond well to treatment. But in some cases, there may be long-term airway damage.
Who is at risk for RADS?
Anyone can get RADS. But you are at higher risk if your job exposes you to irritants. Jobs include:
Diagnosing RADS
If RADS symptoms occur within 24 hours after being exposed to an irritant, see your healthcare provider right away. The provider will ask about your health history and your exposure to irritants. You may have tests done such as:
-
Chest X-ray
-
Breathing test (spirometry)
-
Blood tests such as a complete blood count (CBC) and differential
-
Tests to see the oxygen level in your blood (pulse oximetry or arterial blood gas test)
You may be referred to a healthcare provider who specializes in asthma or allergies. This provider may give you other tests to figure out the best treatment option for you. These tests may include:
Treatment for RADS
Treatment for RADS is the same as treatment for asthma. You will be given medicines to prevent and ease your symptoms. You will also need to stay away from the irritant or any other substances that may trigger your symptoms.
There are different types of asthma medicines. You may need to take more than one. Talk with your healthcare provider to be sure you know how to use all of your medicines correctly. It may be helpful to create an Action Plan for RADS with your provider. This should be updated each year or at provider visits.
Medicines used to treat RADS include:
-
Quick-relief (rescue) medicine. These medicines are fast-acting. They give you quick relief when your symptoms start. They relax and open up the airways. Take these medicines only when needed. Always carry this medicine with you.
-
Long-term control (maintenance) medicine. These medicines help to relax the muscles around your airways. They are often taken on a schedule. Don't skip doses unless your healthcare provider tells you to.
-
Inhaled corticosteroids. These medicines work to reduce airway swelling and inflammation. They are often used when you have more severe symptoms or symptoms that continue. They open up the airways. They are inhaled right into the bronchial tubes of your lungs.
If your symptoms are severe enough, you may also need to take steroids by mouth.
Living with RADS
-
Stay away from the irritant that caused your symptoms. If the exposure occurred at home, switch to a substance or product that is less irritating. If your RADS is job-related, talk with your employer. You may be able to work in the same area if you take your medicine and use safety measures. Talk with your healthcare provider about what kind of safety measures you may need at work. You should also be closely watched to be sure you are not having any breathing issues.
-
If you smoke, stop smoking. Ask your provider for resources to help you quit.
-
Stay away from secondhand smoke.
-
Stay away from other irritants that may trigger your symptoms.
When to call your healthcare provider
Call your healthcare provider right away if you have any of the following:
-
Feeling dizzy, faint, or weak
-
Lasting cough
-
Fast heartbeat or pulse
-
Having trouble doing normal activities
-
Wheezing when you breathe in or out that is different from your normal breathing pattern
-
Wheezing or chest tightness that gets worse, even after taking medicine
Call 911
Call 911 right away if you have any of the following:
-
Trouble walking or talking
-
Fingernails or lips turn blue or gray
-
Trouble breathing
-
Nostrils flare when you breathe
-
With each breath, your chest, ribs, or neck are pulled in
-
You take 30 or more breaths per minute