Understanding Fecal Transplant
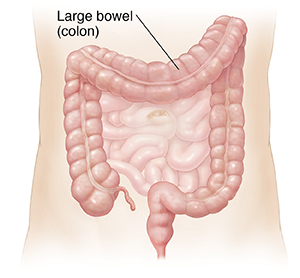
Fecal transplant, also called fecal microbiota transplant (FMT), is used to treat an infection in the large bowel (colon) caused by bacteria called Clostridioides difficile. You may also hear this infection called C. diff. Older people who are in the hospital have a higher risk of getting C. diff. That’s because their ability to fight off germs is lower. But people who haven’t been in the hospital can sometimes get it too. This is called community-acquired C. diff. A fecal transplant may be used when this infection happens over and over again and is severe.
Upsetting the balance
Normally, your large bowel has bacteria living in it. These bacteria are both good and bad.
-
One of the bad bacteria is C. diff. C. diff makes toxins that harm the inside of your large bowel. These toxins make your large bowel become sore and irritated. The result is large amounts of severe diarrhea. Some people with C. diff never get sick, but they can spread the infection to others.
-
The good bacteria help break down food and let nutrients get absorbed. They even help make some vitamins. These good bacteria also keep the bad bacteria from taking over.
So what happens? When you get medicines (antibiotics) for another infection, the medicine helps kill the bacteria causing the infection. But the medicines also kill or limit the work of some of the good bacteria. This changes the balance of the bacteria in your large bowel. With less good bacteria, the bad bacteria grow and take over.
Why fecal transplant is done
A fecal transplant is done to get the bacteria in your large bowel back in balance.
A bowel movement (stool) from a healthy donor has the right balance of good and bad bacteria. This means that there are more good bacteria than bad. This donor stool is given to the person with the infection. As a result, there are more good bacteria to offset the bad. This gets the balance back to what it should be.
How fecal transplant is done
Before a fecal transplant can be done, the bowel movement from a donor is tested to make sure that it’s free of antibiotics and infections. The sample is then made into a form to be used for treatment.
Before you start the fecal transplant procedure, you must sign an informed consent. Signing this document means you understand the risks and benefits of the transplant and other available treatments, and that your questions were answered. Be certain to get answers to all your questions before you sign.
The fecal transplant can be swallowed as capsules or given in a colonoscopy or special enema. The sample can also be given through a tube from the nose into the small intestine. You and your health care provider will decide which method will work best for you.
Here’s a general look at what happens with a fecal transplant. Follow your provider’s specific instructions.
-
Your provider will ask you to identify a donor. Most people choose a family member or close friend.
-
Your provider may want you to take an antibiotic for a week before the procedure. Then you may need to stop taking any antibiotics for about 24 to 48 hours before the transplant. In this case, your last dose would be the day before your procedure.
-
You may be told to take a laxative the night before to make sure that your colon is clear.
-
You may receive directions for not eating or drinking before the procedure, based on which method is planned. Be sure to follow these directions.
-
If the transplant is done with capsules, you'll be told the number of capsules to swallow.
-
You will lie on your side for about 2 hours after the procedure with the transplant in your bowels. You may be given medicine to help slow down your bowels so the transplant stays in place during this time.
-
Your provider will give you instructions about the type of diet and medicines you need to take after the procedure.
Once the procedure is done and you have passed the stool mixture, you can go home. You may need to have more than one treatment as an enema or through the tube over several days.
Risks of fecal transplant
The risks of fecal transplant are most often mild and last only a short time. These may include:
-
Nausea or vomiting (most often with the oral capsules).
-
Belly (abdominal) bloating, pain, or gas.
-
Diarrhea or constipation.
-
A mild fever.
There's a risk that other more serious things may happen. These may be linked to how the transplant was done, such as with a colonoscopy. The risks may include:
-
Effects of sedation.
-
Bleeding.
-
A tear in the colon.
-
Infection.
After the procedure, call your health care provider if you have:
-
A fever of 100.4°F (38°C) or higher, or as directed by your provider.
-
Severe belly pain or bloating.
-
Blood in your stool or vomit.
-
Severe vomiting.
-
Any new or worse symptoms.