Open Kidney Exploration
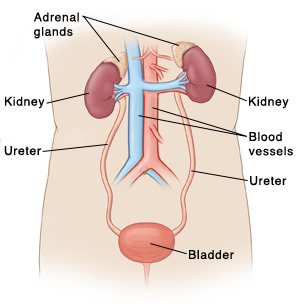
Open kidney exploration is a type of surgery. It's most often done to treat injuries to the kidneys. In rare cases, it may be done to help find the cause of a problem in the kidneys. During the surgery, a cut (incision) is made in your belly (abdomen) or side. The provider treats your kidneys through this incision.
Getting ready for surgery
Follow any instructions from your healthcare provider.
Tell your provider about any medicines you are taking. You may need to stop taking all or some of these before the test. This includes:
-
All prescription medicines
-
Blood-thinning medicines (anticoagulants)
-
Over-the-counter medicines such as aspirin or ibuprofen
-
Street drugs
-
Herbs, vitamins, and other supplements
Follow any directions you are given for not eating or drinking before surgery. This includes coffee, water, gum, and mints. (If you have been instructed to take medicines, take them with a small sip of water.)
The day of surgery
The surgery takes a few hours. You will stay in the hospital for several nights.
Before surgery begins
-
An IV (intravenous) line is placed in a vein in your arm or hand. This supplies fluids and medicines such as antibiotics.
-
You may be given medicine to prevent blood clots.
-
To keep you free of pain during the surgery, you’re given general anesthesia. This medicine allows you to sleep comfortably through the surgery. A tube may be placed in your throat to help you breathe during the surgery.
During surgery
-
The surgeon makes a cut (incision) in your belly (abdomen) or side.
-
The surgeon moves tissues aside to reach your kidneys. They may clamp blood vessels leading to your kidneys. This helps control bleeding.
-
The surgeon repairs any injuries as much as possible. First, the surgeon takes steps to stop any bleeding. Then they clean the injuries. The surgeon removes any damaged tissue. They close the injury area with stitches or other sealing products.
-
If repair can't save your kidney, the surgeon may remove part or all of it.
-
When the surgery is complete, the surgeon closes the skin incision with stitches or staples.
-
A small tube (drain) may be placed near the incision. This drains fluid that can build up after the surgery.
Recovering in the hospital
After the surgery, you will be taken to the PACU (post-anesthesia care unit). There, you’ll wake up from the anesthesia and be closely monitored. You may feel sleepy. You may have an upset stomach (nausea). If a breathing tube was used, your throat may be sore at first. When you are awake and stable, you will be taken to your hospital room. While in the hospital:
-
You will be given medicines to manage your pain. Let your provider know if your pain is not going away.
-
You’ll first get IV fluids. In a day or so, you’ll start on a liquid diet. You’ll then slowly return to a normal diet as tolerated.
-
You’ll be shown ways to cough and deep breathe that can keep your lungs clear and prevent pneumonia.
Recovering at home
After your hospital stay, you will be released to an adult family member or friend. Have someone stay with you for the next few days to help care for you. Recovery time varies for each person. Your provider will tell you when you can return to your normal routine. Until then, follow the instructions your provider gives you. Make sure to:
-
Take all medicines as directed.
-
Care for your incision and drain as instructed.
-
Follow your provider’s guidelines for showering. Don't swim, bathe, use a hot tub, or do other activities that cover the incision with water until your provider says it’s OK.
-
Don't lift anything heavy or do strenuous activities until your provider says it's OK.
-
Don't drive until your provider says it’s OK. Don't drive if you’re taking medicines that make you drowsy or sleepy.
-
Walk a few times a day. Slowly increase your pace and distance, as you feel able.
-
Don't strain to pass stool. If needed, take stool softeners as directed by your provider.
-
Drink plenty of water. This helps prevent urine odor and dehydration.
-
Follow any other diet instructions you’re given. For instance, you may be told to limit the amount of salty foods you eat. You may also need to not drink alcohol, especially if you are still taking prescription pain medicines.
When to call your healthcare provider
Call your healthcare provider right away if you have any of the following:
-
Chest pain or trouble breathing ( call 911 )
-
Fever of 100.4° F ( 38°C) or higher, or as directed by your healthcare provider
-
Symptoms of infection at an incision site. These include increased redness or swelling (inflammation), warmth, more pain, or bad-smelling drainage.
-
Pain that can't be controlled with medicines
-
Nausea or vomiting that won’t go away
-
No urination within 8 hours
-
No bowel movement within 2 days
-
Pain or swelling in your legs
Follow up
You’ll have follow-up visits so your healthcare provider can check how well you’re healing. If your drain, stitches, or staples need to be removed, this will likely be done in 7 days. Going forward, you may need regular visits with your provider. During these visits, you may have routine tests to check how well your kidneys are working.
Risks and possible complications
-
Bleeding (may require a blood transfusion)
-
Infection
-
Blood clots
-
Pneumonia or other lung problems
-
Hernia at the incision site
-
Damage to nearby nerves, blood vessels, soft tissues, or organs
-
Damage to or loss of the affected kidney
-
Kidney or other organ failure
-
Heart attack or stroke
-
Risks of anesthesia. The anesthesiologist will discuss these with you.
Online Medical Reviewer:
Raymond Kent Turley BSN MSN RN
Online Medical Reviewer:
Rita Sather RN
Online Medical Reviewer:
Walead Latif MD
Date Last Reviewed:
12/1/2022
© 2000-2025 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.