Uvulopalatopharyngoplasty (UPPP)
Your health care provider has suggested uvulopalatopharyngoplasty (UPPP) to treat your snoring or sleep apnea (a condition that affects nighttime breathing). During UPPP, the tonsils and soft tissue in the back or sides of the throat, are removed. This helps prevent blockage of the airway during sleep. In many cases, UPPP can permanently improve sleep apnea and decrease snoring. Even so, you may need to continue other treatments such as CPAP (continuous positive air pressure) at first.
Preparing for surgery
Prepare for the surgery as you have been instructed. Tell your health care provider about all medicines you take, especially for obesity and diabetes, or blood thinners. Medicines also include over-the-counter medicines, herbs, and other supplements. You may need to stop taking some or all of them before surgery, as directed by your provider. Also, follow any directions you’re given for not eating, drinking, or smoking before surgery. Tell your provider before your surgery if you have an upper respiratory infection, such as a cold or the flu, fever, or other illness.
The day of surgery
The surgery takes about 60 minutes. If you are having UPPP combined with nasal surgery, your experience will be slightly different than what is described here. In that case, your health care provider can tell you what to expect. Before the surgery is done, you will need to sign an informed consent form. This form shows that you know all of the benefits and risks of the procedure. Be certain all of your questions are answered before you sign the form.
Before the surgery
Here's what to expect before the surgery begins:
-
An IV (intravenous) line is put into a vein in your arm or hand. This line delivers fluids and medicines.
-
You will be given medicine (anesthesia) to keep you free of pain during the surgery. This will likely be general anesthesia, which allows you to comfortably sleep during the surgery.
During the surgery
Here's what to expect at the time of surgery:
-
A special device holds your mouth open. Pillows may be placed under your shoulders and on either side of your neck to support your head.
-
If you still have tonsils, these will likely be removed.
-
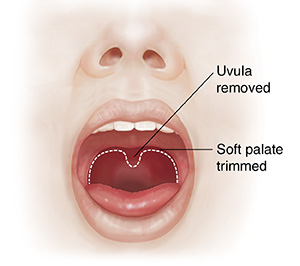
The soft tissue at the back of your mouth (soft palate) is trimmed. The small piece of flesh that hangs down from the soft palate (uvula) is removed.
-
The edges of the remaining tissue are closed with stitches. The stitches dissolve on their own in a few weeks.
-
You may have an injection of local anesthesia. This helps prevent pain after surgery.
Recovering in the hospital
After the surgery, you will be taken to the postanesthesia care unit to be closely kept track of as you wake up from the anesthesia. At first, your throat will feel very sore. It will be hard to talk and swallow. You may also feel sleepy and nauseated. You will receive pain or nausea medicine if needed for comfort. If you have sleep apnea, you will likely stay overnight in the hospital so your breathing can be closely watched. Once you are awake and stable and ready to go home, you will be released to an adult family member or friend who can drive you home.
Recovering at home
Once at home, follow the instructions you have been given. You will have throat pain as you recover. This may come and go. It’s normal for pain to increase a few days after surgery before it starts to improve. It may take around 3 weeks for the pain to go away completely. Eating and drinking will likely be uncomfortable for about 5 days. During your recovery:
-
Take all medicines as directed, including pain medicine.
-
Don't drive while you are on opioid or narcotic pain medicine. Expect to feel sleepy or dizzy while you are taking this medicine.
-
Drink lots of cold liquids. Water, noncitrus juices, and frozen juice bars are good choices.
-
Stick to cold foods and soft foods, which are easiest to swallow. Try ice cream, gelatin, eggs, pasta, and mashed potatoes. Stay away from hot, spicy, acidic, hard, or crunchy foods.
-
Prevent excessive coughing or clearing of your throat for two weeks.
-
Don't use ibuprofen or aspirin for 14 days after surgery, unless your health care provider says it’s OK. You may take acetaminophen as directed for pain.
-
Limit exercise as directed. Your provider will tell you when you can return to your normal activities and routine.
-
Don't lift heavy objects or strain for the first two weeks, or as directed by your provider.
-
Follow instructions for when to start using continuous positive air pressure (CPAP) if it's prescribed.
When to call your doctor
Be sure you have a contact number for your health care provider. After you get home, contact your provider if you have:
-
A fever of 100.4° F ( 38° C) or higher, or as directed by your provider.
-
Any type of bleeding from the mouth or nose.
-
Severe pain not relieved by medicine.
-
Signs of dehydration (dark urine, urinating less often).
-
Inability to eat or drink at all for 2 to 3 days.
-
Other signs or symptoms as indicated by your provider.
Call 911
Call 911 if you have any of the following:
Follow-up
During follow-up visits, your health care provider will check on your healing. A sleep study may be done a few months after surgery. This helps show whether your sleep apnea has improved. If you are still not sleeping normally, other treatments may be needed.
Risks and possible complications
Risks of UPPP include:
-
Bleeding, which may happen a week or more after the surgery (usually needs treatment).
-
Infection.
-
Severe throat pain during the healing period.
-
Changes in the sound of your voice.
-
The feeling that something is stuck in your throat (may last 6 to 12 months).
-
Liquids going into the nose when swallowing.
-
Failure to cure sleep apnea.
-
Risks of anesthesia. You will discuss these risks with the anesthesiologist.