Excisional Biopsy: Neck Lymph Node
The lymph nodes are small bean-shaped structures. They are part of the immune system, which is located all over the body. They are connected to each other by lymph vessels. Lymph nodes filter out waste and harmful substances that are removed from the body. There are a lot of lymph nodes in the neck. These nodes sometimes swell or become enlarged. Then you might be able to feel them under your skin. This swelling is most often caused by infection. But it can also be caused by cancer.
Excisional biopsy helps find the cause of an enlarged lymph node. You may have already had other tests, like imaging scans and a needle biopsy. But in some cases, more tissue is needed to diagnose the problem. During an excisional biopsy, the whole enlarged lymph node is removed. It's then sent to a lab for testing.
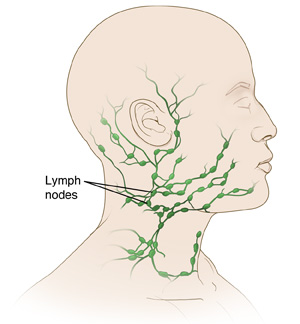 |
| Many lymph nodes are found in the neck area. Your healthcare provider can show you which of your lymph nodes is affected. |
Getting ready for the procedure
Follow the instructions you were given to prepare for lymph node surgery. Be sure to tell your healthcare provider about all medicines you take. This includes over-the-counter and prescription medicines, herbs, vitamins, and other supplements. Also tell them if you use CBD, marijuana, or illegal drugs. You may need to stop taking some or all of these things before surgery. Also follow all directions you are given for not eating or drinking before the procedure.
The day of the procedure
The procedure usually takes about 60 minutes. This is often done as an outpatient procedure. This means you can go home the same day.
Before the procedure starts
Here is what to expect before surgery:
-
A small tube called an IV (intravenous) line is put into a vein in your arm or hand. This tube is used to give you fluids and medicines.
-
A thin needle might be used to inject local anesthesia into the area around the lymph node to numb it. You may also get medicine to sedate you. This will make you relaxed and sleepy. But you'll be able to breathe on your own.
-
Sometimes general anesthesia is used. This lets you comfortably sleep during the procedure. When you have general anesthesia, you may or may not have a breathing tube put in. The tube is attached to a breathing machine (ventilator) during the surgery.
During the procedure
Here's what to expect during the procedure:
-
The skin over the enlarged lymph node is marked and cleaned.
-
A cut (incision) is made into the skin. If possible, the cut is made in the creases of your neck. This makes it less visible when it has healed.
-
The enlarged lymph node is taken out. It's sent to a lab for testing.
-
The incision is closed with stitches, staples, surgical glue, or surgical strips. Then it's bandaged.
-
A tube (drain) might be put in near the incision. This drains out fluids that may build up after the procedure.
After the procedure
You'll be taken to a postanesthesia care unit (PACU). You will be closely watched there as you wake up from the anesthesia. You may feel sleepy and nauseated at first. You'll get medicine to help with any pain or nausea as needed. If you have a drain, you'll be shown how to care for it. When you're ready to go home, have an adult family member or friend drive you. Follow your healthcare provider’s instructions for recovery, such as:
-
Take any prescribed medicine as directed
-
Do deep breathing exercises as instructed
-
Care for your incision, bandage, and drain (if you have one) as advised
-
Try to get up and walk as much as you can
-
Don't do strenuous activity until your provider says it’s OK
When to call your healthcare provider
Call your healthcare provider if you have any of these:
-
Swelling, redness, warmth, or pain in a leg or arm. These could be signs of a blood clot.
-
Fever of 100.4° F ( 38° C) or higher, or as advised by your provider
-
Soreness at the biopsy site that's getting worse
-
Trouble turning your head
-
Any increased redness or swelling, warmth, pain that gets worse, or bad-smelling drainage at the incision site. These could be signs of infection.
-
New bleeding or bruising at the incision site
-
Numbness or tingling in your mouth, jaw, neck, arm, or shoulder
-
Problems speaking or swallowing
-
Hoarse voice that gets worse
Be sure you have a contact number for your healthcare provider. Know how you can reach them after office hours, on weekends, and on holidays if needed.
Call 911
Call 911 if you have:
Follow-up
During follow-up visits, your healthcare provider will check on your healing. If you have a drain, it will likely be removed 1 to 2 days after the procedure as the drainage decreases. Stitches or staples are removed about 7 to 10 days after the procedure. You and your provider will also discuss your biopsy results. If cancer was found, more treatment may be needed.
Risks and possible complications
Risks of this procedure include:
-
Bleeding
-
Infection
-
Injury to the nerves near the lymph node
-
Neck abscess (a pus-filled infection)
-
Scarring
-
Reopening of the incision
-
Another enlarged lymph node
-
Risks of anesthesia. You will discuss these with the anesthesiologist.