Understanding Deep Vein Thrombosis
Deep vein thrombosis (DVT) is a condition in which a blood clot or thrombus forms in a deep vein. A blood clot is most common in the leg. But it can develop in a large vein deep inside the leg, arm, or other part of the body. Part of the clot called an embolus can separate from the vein. It may travel to the lungs and form a pulmonary embolus (PE). This can cut off blood flow to part of the lung or to the entire lung. A PE is a medical emergency and may cause death. Healthcare providers use the term venous thromboembolism (VTE) to describe the 2 conditions, DVT and PE. They use the term VTE because the 2 conditions are very closely related. And, because their prevention and treatment are closely related.
Over time, a blood clot can also permanently damage veins. To protect your health, a blood clot must be treated right away.
How DVT develops
The deep veins of the legs are located in the muscles. These help carry blood from the legs to the heart. When leg muscles contract and relax, blood is squeezed through the veins back to the heart. One-way valves inside the veins help keep the blood moving in the right direction. When blood moves too slowly or not at all, it can pool in the veins. This makes a clot more likely to form.
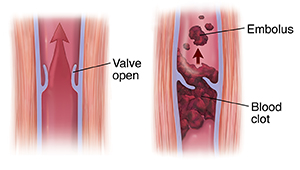 |
| When a muscle contracts, the valve opens. Blood is squeezed toward the heart. When blood moves slowly in a vein, a clot (thrombus) can form. A part of the clot can break off and travel in the bloodstream (embolus). |
Risk factors
Anyone can get a blood clot. These risk factors make a blood clot more likely to happen:
-
Being inactive for a long time, such as when you’re in the hospital, or traveling by plane or car
-
Injured vein due to an accident, a broken bone, or surgery
-
Past blood clots
-
Personal or family history of a blood-clotting disorder
-
Recent surgery
-
Cancer and certain cancer treatments
-
Smoking
Other things can also put you at higher risk for a blood clot. They include:
Common symptoms
A blood clot doesn't always cause obvious symptoms. If you do have symptoms, they often happen suddenly. They may include:
When to call your healthcare provider
Call your healthcare provider if you have any of the common symptoms listed above. In addition, call your provider if you have symptoms of bleeding such as:
-
Blood in the urine
-
Bleeding with bowel movements
-
Bleeding from the nose, gums, a cut, or the vagina
Call 911
Call 911 if you have symptoms of pulmonary embolism such as:
If you take medicine to help prevent blood clots, you have an increased risk of bleeding. Also call 911 if you have heavy or uncontrolled bleeding.
Diagnosing DVT
Your healthcare provider will start with questions about your symptoms and health history along with a physical exam.
Diagnostic tests include:
If your provider thinks you may have pulmonary embolism, more testing will be done.
Treating DVT
Treating a blood clot may include:
Preventing DVT
Many people who are in the hospital are at an increased risk of developing blood clots. So, preventing blood clots is an important part of in-hospital care. The care may include getting out of bed regularly, taking medicine, or using special therapies or devices. Other factors and conditions may increase the risk of blood clots. Review your risk with your healthcare provider.